Residents/Fellows Policies and
Procedures Manual
2024-2025

2
Residents/Fellows Policies and Procedures Manual
MISSION STATEMENT ......................................................................................................................................................................... 6
INSTITUTIONAL COMMITMENT ..................................................................................................................................................... 7
SPONSORING INSTITUTION .............................................................................................................................................................. 9
WELCOME TO GRADUATE MEDICAL EDUCATION .............................................................................................................. 10
DEAN’S OFFICE .................................................................................................................................................................................... 11
ASSISTANT DEANS ............................................................................................................................................................................. 12
GRADUATE MEDICAL EDUCATION OFFICE ............................................................................................................................ 13
CAPITAL AREA HEALTH CONSORTIUM ................................................................................................................................... 15
AFFILIATED HOSPITALS.................................................................................................................................................................. 16
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) COMPETENCIES .................. 19
GRADUATE MEDICAL EDUCATION COMMITTEE (GMEC) ............................................................................................... 21
RESIDENT/FELLOW FORUM ......................................................................................................................................................... 22
SECTION I: HOUSESTAFF INFORMATION .............................................................................. 23
EMPLOYMENT REQUIREMENTS .................................................................................................................................................. 24
APPOINTMENT LETTER/CONTRACT .............................................................................................................................. 25
BACKGROUND CHECK ............................................................................................................................................................. 32
PROFESSIONAL NUMBERS ................................................................................................................................................... 33
STATE LICENSURE/PERMIT REQUIREMENT .............................................................................................................. 37
INSTITUTIONAL CURRICULUM REQUIREMENTS (IC) ....................................................................................................... 38
EMERGENCY LIFE SUPPORT TRAINING ................................................................................................................................... 41
OCCUPATIONAL IONIZING RADIATION EXPOSURE ........................................................................................................... 42
REAPPOINTMENTS PROCESS AND REQUIREMENTS ......................................................................................................... 43
REAPPOINTMENT LETTER/CONTRACT ........................................................................................................................ 44
TRAINING AND EMPLOYMENT VERIFICATION .................................................................................................................... 45
USMLE 3/COMLEX 3 .......................................................................................................................................................................... 46
GRADUATION/SEPARATION REQUIREMENTS ..................................................................................................................... 47
SALARY .................................................................................................................................................................................................... 48
BENEFITS ............................................................................................................................................................................................... 49
PROFESSIONAL LIABILITY/MALPRACTICE INSURANCE AND ADVERSE EVENTS/INCIDENTS ........... 49
TABLE OF CONTENTS

3
Residents/Fellows Policies and Procedures Manual
LONG-TERM DISABILITY ....................................................................................................................................................... 51
WORK-RELATED INJURIES ................................................................................................................................................... 52
SALARY ADVANCE AND ORIENTATION PAY ................................................................................................................ 54
DEPENDENT CARE REIMBURSEMENT ACCOUNT ..................................................................................................... 54
MEDICAL, DENTAL, AND VISION INSURANCE ............................................................................................................. 54
LIFE INSURANCE ....................................................................................................................................................................... 54
TAX-SHELTERED INVESTMENT PROGRAM .................................................................................................................. 55
COBRA INSURANCE COVERAGE CONTINUATION ...................................................................................................... 55
LOAN DEFERMENTS .......................................................................................................................................................................... 55
EDUCATIONAL RESOURCE ALLOWANCE ................................................................................................................................ 56
EDUCATIONAL TRAVEL ................................................................................................................................................................... 58
SECTION II: COMPLIANCE AND INTEGRITY ........................................................................... 59
CONFLICT OF INTEREST/ VENDOR INTERACTIONS .......................................................................................................... 60
HIPAA/PRIVACY AND SECURITY OF CONFIDENTIAL DATA........................................................................................... 64
ACCESSING MEDICAL RECORDS .................................................................................................................................................. 66
PROHIBITION OF DISCRIMINATION AND DISCRIMINATORY HARASSMENT, INCLUDING SEXUAL
HARASSMENT AND SEXUAL ASSAULT, INTIMATE PARTNER VIOLENCE, AND STALKING .............................. 67
FACULTY, STAFF, AND STUDENT RELATIONS ...................................................................................................................... 69
SOCIAL NETWORKING ...................................................................................................................................................................... 70
DRUG-FREE WORKPLACE ACT ..................................................................................................................................................... 72
PROFESSIONAL ATTIRE/DRESS CODE ..................................................................................................................................... 73
DELINQUENT MEDICAL RECORD PROCEDURE .................................................................................................................... 75
SECTION III: PROFESSIONAL ACTIVITIES AND PROFESSIONALISM ......................................... 76
RESIDENT/FELLOW JOB DESCRIPTION ................................................................................................................................... 77
PROFESSIONALISM ............................................................................................................................................................................ 81
COMPACT BETWEEN TRAINEES AND THEIR TEACHERS ................................................................................................ 82
CODE OF CONDUCT ............................................................................................................................................................................ 85
RESIDENTS, FELLOWS, and FACULTY WELL-BEING .......................................................................................................... 87
WORK ENVIRONMENT ..................................................................................................................................................................... 88
CLINICAL AND EDUCATIONAL WORK HOURS RULES/PROCEDURES........................................................................ 90
FATIGUE MITIGATION ...................................................................................................................................................................... 92
TRANSITIONS OF CARE/HANDOVER ........................................................................................................................................ 93
SUPERVISION, PROGRESSIVE AUTHORITY AND RESPONSIBILITY OF RESIDENTS/FELLOWS ..................... 95

4
Residents/Fellows Policies and Procedures Manual
MOONLIGHTINGEXTRA CREDIT .................................................................................................................................................. 99
RESIDENT/FELLOW MISTREATMENT .................................................................................................................................. 101
COUNSELING SERVICES ................................................................................................................................................................ 102
UCONN OMBUDS OFFICE ............................................................................................................................................................. 105
FIT FOR DUTY/EMPLOYEE ASSISTANCE EVALUATIONS .............................................................................................. 106
SECTION IV: PERFORMANCE EVALUATIONS ....................................................................... 109
MILESTONES ...................................................................................................................................................................................... 110
EVALUATION AND PROMOTION .............................................................................................................................................. 111
ACADEMIC DEFICIENCIES REVIEW PROCEDURES .......................................................................................................... 112
CODE OF CONDUCT VIOLATIONS/NON-ACADEMIC DEFICIENCIES REVIEW PROCEDURES ........................ 118
ADMINISTRATIVE LEAVE ............................................................................................................................................................ 125
SECTION V: EMPLOYMENT GUIDELINES AND PROCEDURES ............................................... 126
AFFIRMATIVE ACTION, NON-DISCRIMINATION, AND EQUAL OPPORTUNITY ................................................... 127
PERSONS WITH DISABILITIES/ACCOMMODATIONS FOR DISABILITIES .............................................................. 128
RELIGIOUS ACCOMMODATIONS ............................................................................................................................................... 129
LEAVE POLICY/GUIDELINES ...................................................................................................................................................... 130
VACATION LEAVE .................................................................................................................................................................. 131
SICK LEAVE ............................................................................................................................................................................... 132
LEAVE POLICY OVERVIEW ................................................................................................................................................ 133
GME ONE-TIME LEAVE BANK POLICY .......................................................................................................................... 136
CT FAMILY AND MEDICAL LEAVES OF ABSENCE (CTFMLA), FEDERAL FAMILY AND MEDICAL
LEAVE (FMLA) AND CT PAID FAMILY AND MEDICAL LEAVES OF ABSENCE (CTPFML) ...................... 138
MEDICAL LEAVE ..................................................................................................................................................................... 140
OTHER NON-MEDICAL LEAVE ......................................................................................................................................... 143
MILITARY LEAVE ................................................................................................................................................................... 145
EMERGENCY LEAVE .............................................................................................................................................................. 147
BEREAVEMENT LEAVE ....................................................................................................................................................... 148
PERSONAL LEAVE .................................................................................................................................................................. 149
CONTRACT EXTENSION DUE TO LEAVE GUIDELINES .................................................................................................... 150
RESTRICTED COVENANT ............................................................................................................................................................. 151
CLOSURES AND REDUCTIONS IN PROGRAMS AND PROGRAM SIZE ........................................................................ 152
EXTRAORDINARY CIRCUMSTANCES GUIDELINES ........................................................................................................... 153
SECTION VI: GENERAL INFORMATION AND SUPPORT SERVICES ......................................... 154

5
Residents/Fellows Policies and Procedures Manual
REPORTING CONCERNS ................................................................................................................................................................ 155
AWAY ELECTIVES ............................................................................................................................................................................ 157
OFFICIAL COMMUNICATION WITH THE UNIVERSITY OF CONNECTICUT SCHOOL OF MEDICINE
GRADUATE MEDICAL EDUCATION PROGRAMS ................................................................................................................ 158
MEDICAL TREATMENT/PRESCRIPTION WRITING .......................................................................................................... 159
PROVIDING MEDICAL TREATMENT TO RESIDENTS/FELLOWS ................................................................................ 160
JURY DUTY .......................................................................................................................................................................................... 161
SECURITY ............................................................................................................................................................................................ 162
BEEPERS .............................................................................................................................................................................................. 163
SECURE ELECTRONIC MESSAGING .......................................................................................................................................... 163
MEAL ALLOWANCE......................................................................................................................................................................... 163
HOLIDAY GUIDELINES ................................................................................................................................................................... 164
INCLEMENT WEATHER ................................................................................................................................................................ 165
NEEDLESTICKS & OTHER OCCUPATIONAL EXPOSURE TO BLOODBORNE PATHOGENS .............................. 166

6
Residents/Fellows Policies and Procedures Manual
MISSION STATEMENT
The mission of the University of Connecticut School of Medicine’s Office of Graduate Medical Education
(GME) is to provide effective oversight and management of high-quality, comprehensive, and culturally
relevant educational programs to improve the overall health of the citizens of Connecticut. GME is
committed to providing inclusive clinical learning environments complete with the resources needed to
graduate highly qualified physicians. We do this by promoting academically vigorous programs that foster
physicians’ professional development and prepare skilled, ethical, and compassionate independent
physicians that can meet the challenges of a changing healthcare environment. GME promotes research
and scholarly activity in our residents, fellows, and faculty. We attend to resident well-being and an
inclusive environment where all are treated with mutual respect. Lastly, we collaborate with our affiliated
training sites engaging residents and fellows as integral and transformative members of the health care
community with the goals of providing safe, effective and high-quality care.
Reviewed 4/16, 5/17, 4/19, 3/21, 2/23

7
Residents/Fellows Policies and Procedures Manual
INSTITUTIONAL COMMITMENT
TO GRADUATE MEDICAL EDUCATION
_________________________________________________________________
The University of Connecticut School of Medicine and its governing body, the Board of Directors, has as its
mission the commitment to provide excellent medical education, research endeavors, and medical care to
the citizens of the State of Connecticut and to all others. Graduate Medical Education is identified as a vital
part of this mission. As such, the University of Connecticut School of Medicine sponsors Graduate Medical
Education Programs that train health professionals to practice independently within their specialty. We do
this with integrated partners for graduate medical education comprising John Dempsey Hospital (the
University hospital), Hartford Hospital, Connecticut Children’s Hospital, St Francis Hospital and Medical
Center, and Hospital for Central Connecticut.
The University of Connecticut's School of Medicine sponsors Graduate Medical Education Programs
dedicated to helping and facilitating residents'/fellows’ professional, ethical, and personal development
during residency education. Our graduates are an integral part of the school's efforts to recruit and
maintain the highest quality health professionals to the state.
The Graduate Medical Education Programs, in response to community needs, emphasize primary care
training along with selected specialty programs. Clinical and basic science research opportunities are
encouraged in all areas where there are Graduate Medical Education Programs.
Graduate Medical Education sponsored by the University of Connecticut School of Medicine is dedicated to
the centralization, enhancement, and monitoring of the quality of education provided to residents/fellows
at all participating institutions, as well as to meeting the new demands and responsibilities inherent in
maintaining top quality Graduate Medical Education Programs. We will ensure that the programs meet or
exceed all accreditation, general and specific requirements, from all accrediting bodies such as
Accreditation Council for Graduate Medical Education (ACGME), American Osteopathic Association (AOA),
and American Board of Obstetrics and Gynecology (ABOG). We are also committed to ensuring that
individual residents/fellows are well prepared to meet certification requirements within their specialties.
Each program is dedicated to the development and assessment of each trainee with documentation that
competencies and milestones are met as defined by each specialty. To that end, we have an organized
administrative division that is overseen by the Associate Dean for Graduate Medical Education and Faculty
Affairs and the Graduate Medical Education Committee. In addition, the University of Connecticut School
of Medicine is dedicated to advancing patient care by a supportive educational environment and is
specifically dedicated to the ongoing development and support of our teaching faculty.
To this end, the Governing authorities which include the Board of Directors, Education Council, the Dean
of the School of Medicine, and the administration of the University of Connecticut School of Medicine will
commit educational, financial, and human resources to Graduate Medical Education. Furthermore, the
hospital administration will also comply with the requirements for the Clinical Learning Environment
Review (CLER) visits that focus on patient safety, health care quality, and transitions of care.
8
Residents/Fellows Policies and Procedures Manual
{Signatures on file}
____________________________________________________________
Bruce T. Liang, MD
Dean, School of Medicine
University of Connecticut School of Medicine
Date Signed
____________________________________________________________
Kiki Nissen, MD
Associate Dean for Graduate Medical Education and Faculty Affairs
University of Connecticut School of Medicine
Date Signed
____________________________________________________________
Steven Angus, MD
Designated Institutional Official
University of Connecticut School of Medicine
Date Signed
____________________________________________________________
Janet Widlansky
Executive Director
Capital Area Health Consortium
Date Signed
Revised 2/16, 11/17
Reviewed 11/17, 4/19, 3/21
9
Residents/Fellows Policies and Procedures Manual
SPONSORING INSTITUTION
The University of Connecticut School of Medicine (UConn SOM) is the sponsoring institution for most of
the Graduate Medical Education programs in the Hartford area. The UConn SOM has affiliated with seven
Hartford area hospitals for the education of residents/fellows. These hospitals include Connecticut
Children’s Medical Center, Hartford Hospital/Institute of Living, Hospital for Special Care, John Dempsey
Hospital, St. Francis Hospital and Medical Center, and The Hospital of Central Connecticut. The UConn SOM
must be in good standing with its accrediting organization, the Liaison Committee on Medical Education
(LCME), in order to be successful as a sponsoring institution.
The Graduate Medical Education (GME) Office is part of the University of Connecticut School of Medicine
and is responsible for administering the activities that are common to all of the residency/fellowship
programs. When applicants are selected to join residency/fellowship programs, an appointment
letter/contract is issued by the GME Office.
The GME Office has oversight responsibilities for all residency and fellowship programs. The GME
programs must be in good standing with their accrediting organizations. The majority of the GME programs
are Accreditation Council for Graduate Medical Education (ACGME) accredited programs.
The six affiliated hospitals make up the Capital Area Health Consortium (CAHC). The CAHC has been
contracted by the UConn SOM to be the administrator of salary and benefits for all residency and fellowship
programs; therefore, the CAHC is the official employer of all the residents and fellows. The staff of the CAHC
works closely with the GME Office to ensure that the working conditions for the residents are optimized
and that the pay and benefits are appropriate. CAHC staff participate on Graduate Medical Education
committees. The CAHC Board is made up of representatives from each of the six hospitals. Five of the seven
hospitals are considered major participating institutions. In addition, there are multiple participating
institutions in Connecticut that provide specific learning experiences and are integral to the success of our
Graduate Medical Education Programs.
Revised 4/16, 2/18, 1/23
Reviewed 5/17, 4/19, 3/21

10
Residents/Fellows Policies and Procedures Manual
WELCOME TO GRADUATE MEDICAL EDUCATION
AT THE UNIVERSITY OF CONNECTICUT SCHOOL OF MEDICINE
Graduate Medical Education is the phase of formal medical education beginning at graduation from medical
school and ending after the educational requirements for one of the medical specialties’ certifying boards
have been completed. The objective of graduate medical education is to provide residents/fellows with an
organized educational program in a selected discipline. The goal is to prepare physicians for the
independent practice of medicine. The majority of programs are accredited by the Accreditation Council
for Graduate Medical Education (ACGME) which in turn acts on the recommendations of residency review
committees (RCs) each of which serves a medical or surgical specialty. Specialties’ certifying boards
establish the educational criteria that residents/fellows must achieve to be eligible for board certification.
The University of Connecticut School of Medicine is committed to excellence in education, medical care,
and scholarly pursuits. The emphasis of each program is to facilitate the resident/fellow’s personal and
professional development in six general competencies, and more specifically the achievement of specialty
specific milestones. Residents/fellows are provided guidance and supervision throughout their training
with the goal of providing safe and appropriate patient care.
The University of Connecticut School of Medicine works with five major affiliated hospitals to assume
accountability for the quality of the graduate medical education training programs. The Division of
Graduate Medical Education and the Graduate Medical Education Committee (GMEC) will oversee all
residency and fellowship programs sponsored by the University of Connecticut School of Medicine. Dr.
Steven Angus, Designated Institutional Official, has the authority and responsibility for the oversight and
administration of the GME programs.
We are here to help any resident/fellow should there be concerns about any educational experience or
interaction. All of the GME staff have an open-door policy and welcome you to the University of Connecticut.
Come in for help navigating a problem, to say a quick hello, or to suggest how we can be better!
The Resident/Fellow Policies and Procedures Manual has been developed as a guide and resource for
residents and fellows. Residents/fellows should use this manual as a resource to answer questions
regarding policies and procedures as they arise during their training.
We wish each one of you much success in your training program.
Revised 2/16
Reviewed 5/17, 4/19, 3/21, 2/23
11
Residents/Fellows Policies and Procedures Manual
DEAN’S OFFICE
University of Connecticut School of Medicine
263 Farmington Avenue, AM-047
Farmington, CT 06030-1920
Phone: 860-679-7214
Fax: 860-679-1371
Bruce T. Liang, MD, FACC
Interim Chief Executive Officer, UConn Health
Dean, UConn School of Medicine
Director, Pat and Jim Calhoun Cardiology Center
Ray Neag Distinguished Professor of Cardiovascular Biology and Medicine
Kelly Lester
Executive Assistant to the Dean
Reviewed 4/19, 3/21, 8/22, 2/23
12
Residents/Fellows Policies and Procedures Manual
ASSISTANT DEANS
John Dempsey Hospital
Dr. Scott Allen, Assistant Dean 860-679-2000
sallen@uchc.edu
Tara Rousseau, Administrative Assistant 860-679-4255
Hartford Hospital
Dr. Kenneth J. Robinson, Assistant Dean 860-972-2908
kenneth.robinson@hhchealth.org
Angely D. Martinez, Manager, Medical Education 860-972-4097
angely.martinez@hhchealth.org
St. Francis Hospital (Trinity Health of New England)
Dr. David Shapiro, Chief Medical Officer, Assistant Dean 860-714-7040
dshapiro@trinityhealthofne.org
Sharon Silas, Administrative Assistant 860-714-7029
SSilas@TrinityHealthOfNE.org
Hospital for Central Connecticut
Dr. Jeffrey Finkelstein, Assistant Dean 860-224-5554
jeff.finkelstein@hhchealth.org
Sue Pagano, Executive Assistant 860-224-5640
Susan.Pagano@hhchealth.org
Dr. Steven Hanks, id,
Connecticut Children's Medical Center
Dr. Christine Radar, Assistant Dean 860-545-9366
crader@connecticutchildrens.org
Katherin Lopez, Administrative Assistant 860-545-9366
KLopez01@connecticutchildrens.org
Revised 4/17, 4/19, 10/20, 8/22, 1/23, 11/23
Reviewed 3/21
13
Residents/Fellows Policies and Procedures Manual
GRADUATE MEDICAL EDUCATION OFFICE
University of Connecticut School of Medicine
263 Farmington Avenue, LM-068
Farmington, CT 06030-1921
Phone: (860) 679-2147
Fax (860) 679-4624
https://health.uconn.edu/graduate-medical-education/
Office Hours: 7:00 a.m. – 4:30 p.m.
Kiki Nissen, MD, FACP
Senior Associate Dean for Faculty Affairs
Associate Dean for Graduate Medical Education
Professor of Medicine
860-679-2413
Steven Angus, MD, FACP
Assistant Dean for Graduate Medical Education
Vice Chair of Education for Medicine
Designated Institutional Official
Professor of Medicine
860-679-4420
Wendy Miller, MD, FACP
Assistant Designated Institutional Official
Quality and Safety Education Officer
Associate Professor of Medicine
860-679-4420
Christopher Steele M.D., M.P.H.
Assistant Professor of Medicine
UME/GME Educational Liaison
chsteele@uchc.edu
Martha Wilkie, C-TAGME
Director of Graduate Medical Education
860-679-4458
mhwilkie@uchc.edu
14
Residents/Fellows Policies and Procedures Manual
Melissa Demetro
Finance Manager
860-679-1329
Stephen Bayley
Instructional Design Specialist
(HuskyCT and HealthStream Specialist)
860-679-4295
Carolyn Freer
Administrative Program Coordinator
860-679-2957
Jill Goldsmith, C-TAGME
Administrative Program Coordinator
860-679-4420
Bethany Steinway
Administrative Program Coordinator
860-679-4272
steinway@uchc.edu
Julia Washburn
Administrative Program Assistant 2
860-679-7967
jwashburn@uchc.edu
Revised 6/17, 4/19, 1/21, 3/21, 7/21, 1/22, 8/22, 9/22, 1/23
15
Residents/Fellows Policies and Procedures Manual
CAPITAL AREA HEALTH CONSORTIUM
Your employer, while you are part of the UConn School of Medicine Residency Program, is the Capital
Area Health Consortium (CAHC). They are in The Exchange directly across from the Farmington Avenue
entrance to UConn Health. The Capital Area Health Consortium is a non-profit organized under 501(c)3 of
the Internal Revenue Code.
270 Farmington Ave., Suite 352
Farmington, CT 06032
Phone: 860-676-1110
Fax: 860-676-1303
https://health.uconn.edu/graduate-medical-education/cahc/
Office Hours: 8:30 a.m. – 4:00 p.m.
Michelle Nielson
Executive Director
nielson@uchc.edu
Janet Widlansky
Chief Financial Officer
Michael Tran
Director of Payroll & Benefits
mtran@uchc.edu
Revised 8/22, 11/22, 9/23, 6/24
Reviewed 4/19, 3/21
16
Residents/Fellows Policies and Procedures Manual
AFFILIATED HOSPITALS
UConn Health John Dempsey Hospital
The University Hospital, John Dempsey Hospital provides specialized and routine inpatient and
outpatient services for adults. It is widely recognized for its high-quality care and was named by the
Joint Commission as a top performer in the care of patients with heart failure, heart attack, pneumonia
and surgical needs. UConn’s centers of excellence include:
Geriatrics
Maternal-fetal medicine
Cardiology
Cancer
Orthopaedics
In addition, the John Dempsey Hospital is home to the only full-service Emergency Department in the
Farmington Valley.
Hartford Hospital/Institute of Living
Hartford Hospital is central Connecticut’s leading tertiary medical center with a world-class medical
staff, supported by over 7,000 extraordinary nurses and staff members.
Hartford Hospital is the one of the major teaching hospitals affiliated with the University of Connecticut
Medical School, serving the New England region. With a reputation for providing complex and
innovative care to those in need, Hartford Hospital is built on the foundation of excellence in patient
care, teaching, and research. The Center for Education, Simulation, and Innovation (CESI) is one of the
few Level 1 accredited simulation centers in the United States and is recognized as a leader in
simulation innovation.
Hartford Hospital performed the first successful heart transplant in the state, and pioneered the use of
robotics in surgery. We maintain the only Level 1 Trauma Center in the region, and operate the state’s
air ambulance system, LIFE STAR. We are not the only air ambulance system in Connecticut anymore.
St. Francis Hospital and Medical Center (Trinity Health of New England)
Saint Francis Hospital and Medical Center has been an anchor institution in north central Connecticut
since 1897. In 2015, Saint Francis became part of Trinity Health - New England, an integrated health
care delivery system that is a member of Trinity Health, Livonia, MI, one of the largest multi-
institutional Catholic health care delivery systems in the nation. Saint Francis Hospital and Medical
Center is licensed for 617 beds and 65 bassinets, is a major teaching hospital and the largest Catholic
hospital in New England. Other Saint Francis entities include the Comprehensive Women’s Health
Center, the Connecticut Joint Replacement Institute, the Hoffman Heart and Vascular Institute of
17
Residents/Fellows Policies and Procedures Manual
Connecticut, Smilow Cancer Hospital Yale-New Haven at Saint Francis, and Saint Francis Medical Group.
A regional referral center and major teaching hospital, Saint Francis provides sophisticated,
contemporary medicine with major clinical concentrations in women’s and children’s services,
oncology, cardiology, orthopedics, and rehabilitation.
The Hospital for Central Connecticut
The Hospital of Central Connecticut (THOCC) is a 414-bed, 32-bassinet, acute-care community teaching
hospital with campuses in New Britain and Southington. The hospital was created with the 2006
merger of the former New Britain General and Bradley Memorial hospitals.
Affiliated with the University of Connecticut School of Medicine, The Hospital of Central Connecticut
provides comprehensive inpatient and outpatient services in general medicine and surgery and a wide
variety of specialties. Specialty centers include the Endocrine and Bone Health Center, Cancer Services,
Cardiology, Clinical Research, Family Birthplace, Joslin Diabetes Center Affiliate, Joint and Spine Center,
Psychiatry and Behavioral Health, Sleep Disorders Center, Vascular Center, Center for Bariatric Surgery,
Weigh Your Options Weight Loss Center, Wolfson Palliative Care Consult Services, and Wound Care
Center.
The Hospital of Central Connecticut has a medical staff of more than 400 physicians. Through the
University of Connecticut School of Medicine, the hospital participates in residency programs for
primary care internal medicine, obstetrics and gynecology, otolaryngology, and general surgery.
The Hospital of Central Connecticut is a member of the Central Connecticut Health Alliance, a system of
healthcare affiliates that provides a wide array of services throughout the region, caring for patients
from birth through the end of life.
Connecticut Children's Medical Center
Connecticut Children's Medical Center is a nationally recognized, 187-bed not-for-profit children’s
hospital serving as the primary teaching hospital for the University of Connecticut School of Medicine
department of pediatrics. Connecticut Children’s Medical Center is consistently named among the best
in the nation for several of its pediatric specialties in the annual U.S. News & World Report “Best
Children’s Hospitals” rankings.
The history of Connecticut Children’s spans more than 100 years. Founded as a 10-bed hospital for
children who suffered incurable conditions such as cerebral palsy, spina bifida and polio, Connecticut
Children’s is now one of only two freestanding children’s hospitals in New England—the only
freestanding children’s hospital in Connecticut—that offers comprehensive, world-class health care to
children and adolescents in a patient- and family-centered environment with a focus on research,
education and advocacy.
A comprehensive array of pediatric services is available at our hospitals in Hartford and Waterbury,
with neonatal intensive care units in Hartford (Level 4) and the UConn Health (Level 3), along with a

18
Residents/Fellows Policies and Procedures Manual
state-of-the-art ambulatory surgery center, five specialty care centers and 10 practices across the state
and in Massachusetts.
Our Level 1 Pediatric Trauma Center and Primary Care Center are the busiest between Boston and New
York.
Connecticut Children’s has 2,200 employees with a medical staff of nearly 1,100, practicing in more
than 30 specialties.
The Department of Veterans’ Affairs
The Veterans’ Affairs (VA) Hospital (VA) encompasses an inpatient facility and Ambulatory Care Center
in West Haven; an Ambulatory Care Center in Newington; and six primary care Community Based
Outpatient Clinics.
Affiliation with the University of Connecticut School of Medicine allows the VA Connecticut to
participate in the education and training of more than 600 physicians each year.
Revised 5/17, 4/19, 3/21

19
Residents/Fellows Policies and Procedures Manual
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME)
COMPETENCIES
The University of Connecticut School of Medicine is committed to providing residents/fellows with an
educational environment which allows residents/fellows to successfully demonstrate with satisfaction and
understand the following attributes and objectives set forth by the Accreditation Council for Graduate
Medical Education (ACGME).
Each residency/fellowship program enables its residents/fellows to develop competence in six areas. In
addition, achievable milestones within each competency are defined in program curricula. Towards this
goal, programs define specific knowledge skills and attitudes required and provide the clinical and
educational experiences needed for residents/fellows to demonstrate this competence. As specified in the
ACGME Common Program Requirements, all University of Connecticut School of Medicine sponsored
Graduate Medical Education programs have integrated the general competencies into written curricula
and evaluations related to education and clinical care. Programs use resident/fellow performance data as
the basis for program improvement. Programs are expected to have measurable outcomes to verify
resident/fellow and program performance levels.
The six core competencies as defined by the ACGME are as follows:
1. Patient Care
Residents/fellows must be able to provide patient care that is compassionate, appropriate, and
effective for the treatment of health problems and the promotion of health.
2. Medical Knowledge
Residents/fellows must demonstrate knowledge of established and evolving biomedical, clinical,
epidemiological, and social-behavioral sciences, as well as the application of this knowledge to patient
care.
3. Practice-based Learning and Improvement
Residents/fellows must demonstrate the ability to investigate and evaluate their care of patients, to
appraise and assimilate scientific evidence, and to continuously improve patient care based on constant
self-evaluation and life-long learning. Residents/fellows are expected to develop skills and habits to be
able to meet the following goals:
• identify strengths, deficiencies, and limits in one’s knowledge and expertise;
• set learning and improvement goals;
• identify and perform appropriate learning activities;
• systematically analyze practice using quality improvement methods, and implement changes with
the goal of practice improvement;
• incorporate formative evaluation feedback into daily practice;
• locate, appraise, and assimilate evidence from scientific studies related to their patients’ health
problems;
• use information technology to optimize learning; and,
• participate in the education of patients, families, students, residents/fellows and other health
professionals.

20
Residents/Fellows Policies and Procedures Manual
4. Interpersonal and Communication Skills
Residents/fellows must demonstrate interpersonal and communication skills that result in the
effective exchange of information and collaboration with patients, their families, and health
professionals. Residents/fellows are expected to:
• communicate effectively with patients, families, and the public, as appropriate, across a broad range
of socioeconomic and cultural backgrounds;
• communicate effectively with physicians, other health professionals, and health related agencies;
• work effectively as a member or leader of a health care team or other professional group;
• act in a consultative role to other physicians and health professionals; and,
• maintain comprehensive, timely, and legible medical records, if applicable.
5. Professionalism
Residents/fellows must demonstrate a commitment to carrying out professional responsibilities and
an adherence to ethical principles. Residents/fellows are expected to demonstrate:
• compassion, integrity, and respect for others;
• responsiveness to patient needs that supersedes self-interest;
• respect for patient privacy and autonomy;
• accountability to patients, society, and the profession; and,
• sensitivity and responsiveness to a diverse patient population, including but not limited to diversity
in gender, age, culture, race, religion, disabilities, and sexual orientation.
6. Systems-based Practice
Residents/fellows must demonstrate an awareness of and responsiveness to the larger context and
system of health care, as well as the ability to call effectively on other resources in the system to provide
optimal health care. Residents/fellows are expected to:
• work effectively in various health care delivery settings and systems relevant to their clinical
specialty;
• coordinate patient care within the health care system relevant to their clinical specialty;
• incorporate considerations of cost awareness and risk-benefit analysis in patient and/or
population-based care as appropriate;
• advocate for quality patient care and optimal patient care systems;
• work in interprofessional teams to enhance patient safety and improve patient care quality; and
• participate in identifying system errors and implementing potential systems solutions.
Revised 5/17
Reviewed 4/19, 3/21

21
Residents/Fellows Policies and Procedures Manual
GRADUATE MEDICAL EDUCATION COMMITTEE (GMEC)
The Graduate Medical Education Committee (GMEC) is a standing committee of the School of Medicine. The
GMEC reports to the Education Council of the School of Medicine. The purpose of the GMEC is to oversee
all programs in Graduate Medical Education (GME) sponsored by the University of Connecticut School of
Medicine (UConn SOM). The GMEC is responsible for oversight of all the GME programs sponsored by
UConn SOM in accordance with the Accreditation Council for Graduate Medical Education (ACGME)
institutional requirements and Residency Review Committee (RRC) program requirements. The GMEC
establishes and implements policies regarding the quality of education in the work environment for
residents/fellows at all UConn SOM major affiliated hospitals, partner sites, and GME programs, including
non-accredited programs. The GMEC meets six times a year with written minutes maintained.
Leadership and Membership
The GMEC convenes under the leadership of the Chairperson, the Designated Institutional Official. The
voting membership includes the following:
Designated Institutional Official
Associate Dean for Graduate Medical Education
Assistant Designated Institutional Official
Assistant Deans from five major affiliated hospitals
Department Clinical Chair
Elected Residency Program Directors
Elected Fellowship Program Directors
Quality Improvement/Patient Safety Officer
Executive Director of the Capital Area Health Consortium
Director of Graduate Medical Education
GME Finance Manager
Resident Forum Co-chairs
Residency and Fellowship Program Coordinators
Graduate Medical Education Committee Responsibility
GMEC is responsible for the oversight of the ACGME accreditation status of the sponsoring institution and
each of its programs, the quality of the GME learning and working environment at all participating sites,
the quality of the educational experience in each program, ACGME annual program evaluations and self-
studies, implementation of new policies for vacation and leaves of absence; including medical parental, and
caregiver leaves of absence, all processes related to reductions and closures of programs, individual sites,
and the sponsoring institution. GMEC is also responsible for the review and approval of new programs,
new program directors, ACGME progress reports, program complement changes and resident/fellow
stipends and benefits, and new educational initiatives.
Revised 4/17, 2/23
Reviewed 4/19, 3/21

22
Residents/Fellows Policies and Procedures Manual
RESIDENT/FELLOW FORUM
The Resident/Fellow Forum is a committee for residents/fellows in all programs. The members are
selected by their peers each academic year. All programs are invited to send one or more representatives
to the Forum, which meets every other month. Program Directors are informed about the meetings so that
residents/fellows may be released from other responsibilities. The resident/fellow representatives select
a member to chair or two members to co-chair and convene the meetings. Representatives from the
Graduate Medical Education Office and the Capital Area Health Consortium may be invited to spend 15-20
minutes at the beginning of the meeting with the Forum members so that administrative questions can be
answered. The group then meets on its own to discuss issues that cross disciplines and sites.
A Resident/Fellow Forum report is a standing GMEC agenda item.
Revised 2/16, 5/17
Reviewed 4/19, 3/21

23
Residents/Fellows Policies and Procedures Manual
SECTION I: HOUSESTAFF INFORMATION
24
Residents/Fellows Policies and Procedures Manual
EMPLOYMENT REQUIREMENTS
The following must be completed for residents/fellows to begin employment, and training in any
residency/fellowship program sponsored by the University of Connecticut School of Medicine:
Signed Appointment Letter/Contract
Cleared Background Check
Completion of Institutional Curriculum (IC)
Connecticut State Permit
Copy of the resident/fellow’s ECFMG certificate, if applicable
Copy of the resident/fellow’s medical school diploma
Professional numbers enrollment
Participation in orientation
Pre-employment physical screening including immunization documentation and pre-employment drug
screening
Respirator fit test
Valid Social Security number (J1 residents/fellows within 4 weeks of start date)
Valid visa/employment status
Revised 4/17, 4/19, 3/21
25
Residents/Fellows Policies and Procedures Manual
APPOINTMENT LETTER/CONTRACT
Date: Program:
Name: Post-Graduate Year Level:
Address: Duration of Appointment:
Current Salary at this Level:
This includes the amount for your orientation period.
By signing and returning the final page of this appointment letter, thus accepting this offer, you receive an
appointment with the University Of Connecticut School of Medicine (UConn SOM), the Sponsoring
Institution of your program, and become an employee of the Capital Area Health Consortium (CAHC). Your
employment with the CAHC does not alter your relationship with your residency/fellowship program and
is expressly contingent upon you remaining in good standing in your program. All decisions about the
academic aspects of your program will be governed by your Program Director and the Graduate Medical
Education (GME) Office. Your appointment is also governed by all of the UConn SOM policies, privileges,
procedures, and responsibilities outlined in the accompanying material, your program’s manual, and the
Residents/Fellows Policies and Procedures Manual (Manual). The Manual, including the Code of Conduct,
is available at https://health.uconn.edu/graduate-medical-education/resident-fellow-policy-manual/. A
copy can also be obtained from your Program Coordinator or the GME Office personnel.
This appointment is contingent upon you successfully completing all prerequisites which may include
medical school or residency/fellowship; passing a pre-employment screening, providing documentation of
meeting all required vaccines recommended for healthcare workers, including COVID-19 vaccination
(vaccines will be provided to you if necessary), passing a drug screening test (including screening for
marijuana), passing a criminal background check, and providing appropriate United States Medical
Licensing Exams (USMLE), Comprehensive Osteopathic Medical Licensing Examination (COMLEX), or
equivalent examination; and completing other employment requirements listed in the Manual. Please read
this appointment letter carefully and contact your Program Coordinator or the GME Office personnel with
any questions you may have.
Continuous training is vital to all residency and fellowship programs. Continued status in your academic
program is required for this appointment to remain active. Termination from your academic program will
terminate this appointment and your CAHC employment. Reasons that may terminate this appointment
and any obligations the UConn SOM has to you shall include, but are not limited to, failure to meet
employment requirements, failure to satisfy the academic requirements of the program; failure to progress
in knowledge or performance at a satisfactory rate; failure to attain or demonstrate competence in any of
the six Accreditation Council for Graduate Medical Education (ACGME) competencies; failure to meet the
requirements for continuous training; or conduct unbecoming a physician or otherwise in violation of the
Code of Conduct.
Appointments to subsequent PGY years will be made at least four months prior to your current
appointment end date. Reappointment and/or promotion will be based on each program’s appraisal of
performance in the six Accreditation Council for Graduate Medical Education (ACGME) competencies,
specialty-specific milestones and program specific requirements.

26
Residents/Fellows Policies and Procedures Manual
If your Program Director determines a reappointment/promotion will not occur within the four months
prior to the end of the appointment, written notice will be provided as circumstances reasonably allow.
Reappointment that does not occur as expected may be grieved according to the Academic Deficiencies
Review Procedures and Code of Conduct Violations/Non-Academic Deficiencies Review Procedures in the
Manual.
In the event of a national disaster, act of war, civil unrest, or other causes beyond the control of any party
that may disrupt the ability of the program to operate, this appointment may be suspended or terminated
in accordance with the Extraordinary Circumstances Guidelines in the Manual.
UConn SOM’s Responsibilities
UConn SOM has a responsibility to provide:
An academic program that meets the educational needs of residents/fellows including the
opportunity to acquire the skills, attitudes, and knowledge consistent with proper patient care
Patient care ancillary services, medical records, and other support services necessary for quality
patient care
Readily available faculty supervision
Professional liability insurance coverage for activities within the scope of your training program
and period of participation, and afterwards, for claims arising out of medical incidents that
occurred during the period of your program participation
A clinical and educational work hour policy consistent with patient safety and the ACGME
Institutional and Program-Specific Requirements
Oversight of the program and resident/fellow compliance with both the ACGME Institutional and
Program-Specific Requirements
A work environment that includes adequate food services, safe on-call sleeping quarters, and an
overall environment of safety and security
Written policies including, but not limited to: Accommodations For Disabilities; Evaluation;
Academic Deficiencies Review Procedures and Code of Conduct Violations/Non-Academic
Deficiencies Review Procedures; Moonlighting/Extra Credit; Rotation-Specific Clinical and
Educational Work Hours; Leaves; Supervision; Counseling Services; Prohibition of Discrimination
and Discriminatory Harassment, Including Sexual Harassment and Sexual Assault, Intimate
Partner Violence, and Stalking; and Work Environment
Reappointment letters of agreement if you meet the academic standards and curriculum
requirements of the program
Further details of the above are available in the Manual.
Program Responsibilities
The program has a responsibility to:
Meet its educational goals as they are described in its program manual/curriculum and on the
forms submitted to the specific ACGME Residency Review Committee (RC) or equivalent. The
goals and the outlines of the usual resident/fellow assignments for each year, which may involve
activities in several hospitals, are available in the program office or internet-based educational
system such as HuskyCT. A username and password will be provided by Program at the beginning
of training. The Program Director or designee may find it necessary to modify resident/fellow
assignments as required by available personnel, education resources, institutional patient care
27
Residents/Fellows Policies and Procedures Manual
responsibility, career goals, and academic progress of each resident/fellow
Provide timely evaluations to residents/fellows about their performance in all aspects of the
program
Follow institutional policies for grievance and due process for any academic or non-academic
disciplinary action taken. See policies on Academic Deficiencies Review Procedures and Code of
Conduct Violations/Non- Academic Deficiencies Review Procedures in the Manual
Abide by accreditation standards. Most residency/fellowship programs under UConn SOM are
accredited by the ACGME and the discipline specific RC or similar organizations. Non-ACGME
accredited programs are required to meet similar standards, policies, and procedures as the
accredited programs. Residents/fellows in all programs are required to abide by all policies and
procedures in the Manual
Design a curriculum in which residents/fellows who perform satisfactorily will be able to meet
board certification requirements for their discipline if applicable
Make information about specialty board certification requirements available in the program
office or internet-based educational system such as HuskyCT. You may also contact the GME
Office to request board certification requirements
Provide reasonably timely notice of the effect of leave(s) of absence on the ability of
residents/fellows to satisfy requirements for program completion and, if possible, board
eligibility requirements
Certify to the discipline specific board that each individual resident/fellow has or has not met all
requirements
Monitor resident/fellow adherence to clinical and educational work hour standards
Make reasonable efforts to monitor stress, fatigue in residents/fellows, and provide information
on available support services
Resident/Fellow Responsibilities
Accordingly, you are expected to:
Perform all duties and accept all assignments designated by the program director or designee.
Your performance will be evaluated by faculty, your program director, and others as may be
required
Acknowledge personal responsibility for understanding and accepting the requirements of the
discipline in which you are training
Be able to perform satisfactorily, with or without reasonable accommodation, in all required
components of your program. See the Accommodations for Disabilities policy for further details
in the Manual.
Develop a personal program of self-study and professional growth with guidance from the
teaching faculty and staff
Demonstrate competency in the areas of patient care, medical knowledge, communication and
interpersonal skills, professionalism, practice-based learning and improvement, and systems-
based practice for the discipline you are in
Participate in safe, effective, and compassionate patient care, commensurate with your level of
advancement and competence, under the general supervision of appropriately privileged
teaching faculty and staff
Participate fully in the educational and scholarly activities of your program and, as required,
assume responsibility for teaching and supervising other residents/fellows and students
Participate in programs and activities involving the medical staff and adhere to established

28
Residents/Fellows Policies and Procedures Manual
practices, procedures and policies of the training site
Participate in committees and councils, especially those that are related to patient care review
activities
Develop an understanding of ethical, socioeconomic and medical/legal issues that affect GME and
how to apply cost-containment measurements in the provision of patient care
Submit accurate documentation of duty hours, confidential written evaluations of the faculty, the
program, and other information as may be required
Become familiar with the Manual, comply with, and be subject to all policies and procedures set
forth in the Manual including, but not limited to: Accommodations For Disabilities; Evaluation;
Academic Deficiencies Review Procedures and Code of Conduct Violations/Non-Academic
Deficiencies Review Procedures; Moonlighting/Extra Credit; Rotation-Specific Clinical and
Educational Work Hours; Leaves; Supervision; Counseling Services; Prohibition of
Discrimination and Discriminatory Harassment, Including Sexual Harassment and Sexual
Assault, Intimate Partner Violence, and Stalking; and Work Environment
Abide by all rules, regulations, and bylaws of the program, clinical department, and institution in
which they are assigned including standards required to maintain accreditation by relevant
accrediting, certifying, or licensing organizations, attaining and maintaining authorization to
work in the United States, and a valid training permit in the State of Connecticut throughout the
duration of this appointment
Become familiar with, comply with, and be subject to all site policies, rules, and regulations; state,
federal and local laws; and standards required to maintain accreditation by relevant accrediting,
certifying, or licensing organizations, including attaining and maintaining authorization to work
in the United States and a valid training permit in the state of Connecticut throughout the
duration of this appointment
Consent to and pass a pre-employment criminal background check and a pre-employment drug
screening test that includes screening for marijuana, as well as complete other employment
requirements
Return all hospital properties such as books, beepers and equipment; complete all records; and
settle professional and financial obligations prior to departing from your training program,
UConn SOM, and sites
Be of good moral and ethical character. Residents must demonstrate an understanding of their
personal role in the safety and welfare of patients entrusted to their care and the assurance of
their fitness for work, including: management of their time before, during, and after clinical
assignments; and, recognition of impairment, including from illness, fatigue, and substance use,
in themselves, their peers, and other members of the health care team.
Demonstrate sufficient confidence to enter practice without direct supervision in order to
satisfactorily complete the training program
Report any of one’s own activity or behavior that results in a police investigation or an arrest or
that receives media attention such that the safety of patients or the reputation of the University
could be compromised
Capital Area Health Consortium Responsibilities:
Provide salaries and reimburse educational and travel allowances as outlined in the Manual
Provide health, dental, life, and disability insurance as outlined in the Manual
Provide counseling services including services for and assessment of physical impairment and
substance abuse for residents/fellows through UConn Health’s Employee Assistance Program,
29
Residents/Fellows Policies and Procedures Manual
confidential contracted mental health providers and/or the Health Assistance Intervention
Education Network (HAVEN) as appropriate
Provide written policies on family and medical leaves and other leaves of absence (with or without
pay) from employment to include personal and sick leave consistent with applicable laws and
communicate with residents about the same
Benefits
Benefits described are based on the information at the time this appointment is issued. See the Manual for
further details. Medical, dental, and vision insurance is effective on July 1 for all academic year hires. For
off-cycle start dates, coverage begins on the day of hire. The consortium will provide information regarding
interim insurance coverage should a resident/fellow need coverage prior to July 1. For all J-1 exchange
visitors and accompanying J-2 dependents coverage will be in accordance with the U.S. Code of Federal
Regulations (22 CFR 62.14).
There is a bi-weekly payroll deduction for health insurance (medical $17.50, dental $5, and vision
$1.85) and a discounted price for adding family members to your coverage
Life insurance is at no cost to you
Long Term Disability insurance is at no cost to you
Counseling services through UConn’s EAP and contracted mental health providers are at no cost
to you
The following paid leave per twelve months (no leave can be carried over)
• Four weeks’ vacation (one week equals five days + two weekend days)
• Ten sick days for one's own illness
• Up to 12 Weeks (84 days) for medical leave for own disability/illness, with a health provider’s
note after meeting eligibility requirements. All available paid sick and vacation time (with the
exception of two weeks of vacation time which will be reserved) must be used first. A health
provider’s note is required to return.
• Paid family leave is defined by Connecticut State law and paid at a maximum weekly rate that
varies with the minimum wage rate. Eligibility can be up to 12 weeks (84 days). Available sick
and vacation time must be used first (with the exception of two weeks of vacation time which
will be reserved).
• Administrative Leave
• If training is extended for any reason, vacation granted during an extension will vary and
depend on the amount of extension required to complete the requirements of training
Unpaid Leave with Program Director’s permission
• Personal Leave
• Unpaid family and medical leave as defined by Connecticut State law. Eligibility can be up to 12
weeks. Available sick and vacation time must be used (with the exception of two weeks’
vacation time which will be reserved). Leaves for military active or reserve service and spousal
military leaves will be granted in accordance with the various Federal laws.
Any extended leaves or multiple absences may result in additional time in the program and
extension of your appointment. See Contract Extension Due to Leave in the Manual.
Professional liability coverage. You are covered while you are carrying out assigned duties as part
of your residency/fellowship training program including protection for claims filed after
completion of your residency/fellowship program. Professional activities outside the program are
not covered.

30
Residents/Fellows Policies and Procedures Manual
Further detailed information is available in the Manual.
Moonlighting/Extra Credit
With written permission from your Program Director or designee, you may engage in professional
activities to the extent that such activities do not interfere with your health, performance, or clinical
and educational work hour requirements. It is your responsibility to obtain licensure, liability
coverage, and narcotic registration for use in moonlighting not related to your residency/fellowship
program. See the Manual for further details.
Evaluation of Resident/Fellow, Residency/Fellowship Program
As the position of resident/fellow involves a combination of supervised, progressively more
complex, and independent patient evaluation and management functions and formal educational
activities, your competence is evaluated on a regular basis. The program maintains a confidential
record of your evaluations.
Evaluations of your progress will be conducted according to UConn SOM’s Policy on Evaluation in
the Manual. In addition, you are expected to participate in the evaluation of your
residency/fellowship program. This includes the submission of a written evaluation of each clinical
rotation and key teaching faculty on each rotation following completion of each rotation.
In the event of any action against you related to academic or any other deficiencies which could
jeopardize normal progress towards completion of your residency/fellowship program, your rights
are protected under UConn SOM’s policies on Academic Deficiencies Review Procedures and Code
of Conduct Violations/Non- Academic Deficiencies Review Procedures in the Manual.
Pre-Employment Physical/Fit to Work Status
You are required to provide adequate documentation and attain a pre-employment screening to
ascertain immunizations to communicable diseases in accordance with University and the
University’s School of Medicine policies and state law. This includes vaccination against COVID-19.
The required immunization must be maintained and updated as needed during the entire period of
your residency/fellowship training, including annual TB skin testing or prescribed testing. You will
be required to have a negative drug screening test that includes screening for marijuana prior to
beginning your training or employment.
Institutional Curriculum
The Institutional Curriculum was designed to provide a curriculum that is universal to all programs
and reflects either RC requirements or hospital/Joint Commission requirements. By providing an
Institutional Curriculum, hospital administrative offices are guaranteed that residents/fellows meet
credentialing aspects. Some courses are required to be completed prior to starting, some courses
will be completed annually, and some courses will need to be completed once during a residency or
fellowship period. Other than the required pre-employment and annual courses, it is decided by the
programs how often and when the other courses will be completed and their requirements are
compulsory. Most of the courses are online. Further details are available in the Manual.
Sign and Return

31
Residents/Fellows Policies and Procedures Manual
On behalf of UConn SOM’s GME Office, the CAHC, and training sites, we would like to welcome you. We are
pleased that you will be joining us for your residency/fellowship training program.
Sincerely,
Steven Angus, MD, FACP
Designated Institutional Official
I hereby certify all information provided by me in my application for a position in a UConn SOM
residency/fellowship program and provided by me in the course of applying for a position in the
residency/fellowship training program at UConn SOM is truthful and accurate. I further understand that if
it is discovered that any information provided by me on the application or any of the other information
provided by me in the course of applying for a residency/fellowship position at the University of
Connecticut School of Medicine is found to be false, untruthful or misleading, I will be subject to immediate
cancellation of this appointment and terminated from employment if employment has begun. I also
understand that I may be required to cover additional shifts, beyond what is required as part of my
program’s back-up or jeopardy policy (for which there is no additional compensation), and if I cover
additional shifts, I will receive additional compensation proportionate to the number of shifts covered up
to $30,000.
I accept the offer to become an employee of the CAHC and the appointment as a resident/fellow with UConn
SOM. I agree to abide by the conditions set forth in this appointment letter and agree to complete the full
term of appointment. I also attest to abide by all policies pertaining to my training and employment as
outlined in this appointment letter and expanded upon in the Manual. I also acknowledge that the Manual
is subject to change and it is my responsibility to comply with the current policies that are set forth in the
Manual. This includes all changes made to policies, procedures, and benefits that may have happened since
applying to a residency/fellowship program at UConn SOM.
____________________________________________________________ ______________________
Name
Date
Revised 2/16, 5/17, 9/18, 3/21, 5/22, 2/23, 6/24
Reviewed 4/19, 2/21

32
Residents/Fellows Policies and Procedures Manual
BACKGROUND CHECK
The Graduate Medical Education Committee requires that every resident/fellow pass a criminal
background check including a government sanctions check in order to train in a residency/fellowship
program.
The Police Department at UConn Health will be responsible for conducting this background check. The
Capital Area Health Consortium (CAHC) will pay the fee for this service.
Revised 4/17, 3/21
Reviewed 4/19, 2/23
33
Residents/Fellows Policies and Procedures Manual
PROFESSIONAL NUMBERS
Residents/fellows are required to register for a variety of numbers to ensure proper patient care can be
maintained. The next several pages will explain these numbers.
These are the first 2 registrations that need to be completed.
National Provider Identifier (NPI) Number – residents will receive instructions from GME Office
regarding how to complete this enrollment
Connecticut Controlled Substance (CSR) Number – residents will receive instructions from GME
Office regarding how to complete this enrollment
Then, this registration needs to be completed with a valid NPI number
Connecticut Medicaid Assistance Program (CMAP) – GME Office will complete this enrollment on
behalf of the resident
Finally, complete this registration with a valid CSR and hospital DEA number
Connecticut Prescription Monitoring and Reporting System (CPMRS) – GME Office will complete
this enrollment on behalf of the resident
Drug Enforcement Administration (DEA) Number – GME Office will complete this enrollment on
behalf of the resident
Revised 4/17, 3/21, 2/23
Reviewed 4/19
34
Residents/Fellows Policies and Procedures Manual
National Provider Identifier (NPI) Number
A National Provider Identifier (NPI) is a unique 10-digit identification number issued to health care
providers in the United States by the Centers for Medicare and Medicaid Services (CMS). All
residents/fellows are required to apply for and receive a NPI number at the time of training.
Residents/fellow must have an NPI before starting training at UConn with the appropriate taxonomy and
program address. Failure to comply with this requirement could result in a resident’s/fellow’s inability to
prescribe medications and begin training, employment and benefits. The University of Connecticut School
of Medicine will not be responsible for any loss of privileges or fines as the result of the resident/fellow’s
failure to comply with the above mandate.
Please follow the instructions below and call the GME Office with any questions:
If a resident/fellow has not applied for a NPI and they have a Social Security Number, they should
complete the online application at: https://nppes.cms.hhs.gov/NPPES/NPIRegistryHome.do
If a resident/fellow has not applied for a NPI and they do not have a Social Security Number, they
must complete the paper application available at:
http://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/Downloads/CMS10114.pdf
If a resident/fellow is coming to a UConn sponsored program and already has an NPI, they must
change the business address of the previous NPI number to their new program’s mailing address
(please contact your program for this information). The taxonomy should be “390200000X –
Student in an Organized Health Care Education/Training Program”, unless they have a Connecticut
State Medical License that will be maintained throughout employment as a resident/fellow and are
practicing independently in the state of Connecticut.
o Information can be changed online at:
https://nppes.cms.hhs.gov/NPPES/StaticForward.do?forward=static.npistart
o Information can be changed with a paper application (could take 4-6 weeks) available at:
http://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/Downloads/CMS10114.pdf.
Revised 4/17
Reviewed 4/19, 3/21, 2/23
35
Residents/Fellows Policies and Procedures Manual
Connecticut Controlled Substance Number (CSR)
The State Department of Consumer Protection mandates that all residents/fellows practicing in the State
of Connecticut must be registered to prescribe any controlled substance to any patient. This is different
than the Federal DEA number as this is a State regulation. As long as the resident/fellow is employed by
the Capital Area Health Consortium, the Capital Area Health Consortium (CAHC) will cover the registration
fee.
All new incoming residents/fellows will submit their paperwork prior to beginning training and
employment. If you already have an active CT Controlled Substance number when you join your UConn
program, please inform the GME office. After the initial registration, all residents/fellows will be notified
by the State of Connecticut when renewal is required. Residents/fellows are required to renew their
registration every odd-numbered year. The CAHC will reimburse the resident/fellow via their paycheck. A
copy of the payment must be provided to the resident’s/fellow’s Program Coordinator before the
reimbursement can be processed.
All physicians are required to notify the State of Connecticut Department of Consumer Protection License
Services Division at 165 Capitol Ave., Hartford, CT 06106 within five (5) days of a change in address or
department.
Failure to comply with this requirement could result in a resident’s/fellow’s inability to prescribe
controlled substance medications and may also result in a fine. The CAHC and the University of Connecticut
School of Medicine will not be responsible for any loss of privileges or fines as the result of the
resident’s/fellow’s failure to comply with the above mandate.
Revised 4/17
Reviewed 4/19, 3/21, 2/23
Connecticut Medicaid Assistance Program (CMAP)
The Department of Social services (DSS) provides medical assistance to low-income people through the
Connecticut Medical Assistance Program (CMAP). All residents/fellows are required to register with the
Connecticut Medicaid Assistance Program (CMAP). Patients are dependent on the enrollment of
residents/fellows to receive benefits such as a prescription.
The CMAP enrollment requires the resident/fellow to have a National Provider Identifier (NPI) before
registering. Once the NPI number is obtained, a resident/fellow should apply to CMAP at
www.ctdssmap.com.
Failure to comply with this requirement could result in a resident’s/fellow’s inability to prescribe. The
University of Connecticut School of Medicine will not be responsible for any loss of privileges or fines as
the result of the resident’s/fellow’s failure to comply with the above mandate.
Revised 4/17
Reviewed 4/19, 3/21, 2/23

36
Residents/Fellows Policies and Procedures Manual
Connecticut Prescription Monitoring and Reporting System (CPMRS)
The purpose of the Connecticut Prescription Monitoring and Reporting System (CPMRS) is to present a
complete picture of a patient’s controlled substance use, including prescriptions by other providers, so that
the provider can properly manage the patient’s treatment, including the referral of a patient to services
offering treatment for drug abuse or addiction when appropriate. This is managed by the Connecticut
Department of Consumer Protection.
A Connecticut Controlled Substance Number is required to register with the CPMRS at www.ctpmp.com.
Failure to comply with this requirement could result in a resident’s/fellow’s inability to prescribe
medications and may also result in a fine. The University of Connecticut School of Medicine will not be
responsible for any loss of privileges or fines as the result of the resident’s/fellow’s failure to comply with
the above mandate.
Revised 4/17
Reviewed 4/19, 3/21
Drug Enforcement Administration (DEA) Number
A Drug Enforcement Administration Number allows a health care provider to write prescriptions.
Residents/fellows are provided with a DEA Number specific to each affiliated hospital referred to as the
institutional DEA number. No application is needed for an institutional DEA number to be issued. This is
not an individual DEA. The individual DEA number can be obtained after a physician applies for and
receives a state medical license. The individual DEA number stays with the physician throughout his/her
career. A resident/fellow that wants to moonlight must have a state medical license and an individual DEA
Number.
The resident/fellow must use the specific hospital DEA and suffix where the resident/fellow provided
patient care to the patient. In other words, if a patient is seen at JDH and a resident/fellow writes a
prescription for that patient, then the resident/fellow must use the DEA provided by JDH, plus their JDH-
specific suffix.
Each Medical Education office at the affiliated hospitals will provide institutional DEA numbers for that
hospital when a resident/fellow starts or participates in an orientation at that site.
Revised 4/17
Reviewed 4/19, 3/21, 3/23

37
Residents/Fellows Policies and Procedures Manual
STATE LICENSURE/PERMIT REQUIREMENT
The State of Connecticut requires all residents/fellows to have a Connecticut State Permit. The Graduate
Medical Education (GME) Office designee will obtain the permit for all residents/fellows. No application
by the resident/fellow is needed. The permit is issued by the State of Connecticut Department of Public
Health. The resident/fellow does not receive the permit. CT resident permit numbers can be looked up
here.
A Connecticut State medical license is not required to participate in most residency/fellowship programs.
Residents/Fellows should refer to their program’s licensure policy in the program’s manual. A
resident/fellow that obtains a Connecticut medical license and participates in a program that does not
require a medical license, will do so at their own expense.
Reviewed 4/17, 4/19, 3/21, 2/23

38
Residents/Fellows Policies and Procedures Manual
INSTITUTIONAL CURRICULUM REQUIREMENTS (IC)
The Institutional Curriculum (IC) was designed to provide a curriculum through Healthstream that is
universal to all programs. These required courses are to be completed prior to orientation. The GME Office
will sign you up with an account for Healthstream. For questions, please contact Steve Bayley
Orientation Day 1 (if you miss orientation, you will be assigned a course on Healthstream)
Incoming Courses – Courses that must be completed before residents/fellows can begin. These courses
are automatically assigned in Healthstream. Approximately 12 hours to complete all courses.
Compliance/Regulatory
Active Assailant Training (6 min)
A Lesson in Phishing (5 min)
COVID 19 General Information on Infection Control (20 min)
Emergency Notifications-Plain Language (5 min)
Office of Healthcare Compliance & Privacy Training and IT Security (45 min)
Informed Consent (45 min)
OR Fire Safety/ Electrosurgery & The Bovie (Anesthesiology, Neurosurgery, OBGYN,
Orthopedics, Hand Surgery, Pediatric Orthopedics, Orthopedic Spine Surgery, Orthopedics
Sports Medicine, Otolaryngology, Surgery, Surgical Critical Care, Pediatric Surgery, Vascular
Surgery, Maternal Fetal Medicine, Reproductive Endocrinology, Acute Care, Pediatric
Anesthesiology, Minimally Invasive Gynecologic Surgery)
Radiation Safety (Anesthesiology, Pediatric Anesthesiology, Otolaryngology, Pediatric
Otolaryngology, Orthopedics, Pediatric Orthopedics, Radiology, Surgery, Pediatric Surgery,
Urology, Acute Care Surgery, Cardiology, Endocrinology, Pediatric Endocrinology,
Interventional Cardiology, Gastroenterology, Pediatric Gastroenterology, Orthopedic
Surgery, Orthopedic Hand Surgery, Orthopedic Shoulder and Elbow, Orthopedic Spine
Surgery, Pulmonary Critical Care, Vascular Surgery, Neurosurgery)
Safe and Effective Process to Prepare Items for Sterilization (Emergency Medicine, Family
Medicine, Interventional Cardiology JDH, Pulmonary Critical Care, OBGYN, Orthopedics
Sports Medicine, Otolaryngology, Neonatology, Radiology, Surgery, Urology, Maternal Fetal
Medicine, Reproductive Endocrinology, Minimally Invasive Gynecologic Surgery, Emergency
Medicine - International Disaster)
Sexual Harassment Training (120 min)
Standard Precautions: Bloodborne Pathogens and other Potentially Infectious Material (55
min)
Workplace Violence (30 min)
Patient Care
Abuse and Neglect: Identification, Assessment and Response (15 min)
Elder Abuse (30 min)
Incarcerated Patient Med Surg 5 Training (10 min)

39
Residents/Fellows Policies and Procedures Manual
Interpreter Services at UConn Health (15 min)
Moderate Sedation/Analgesia (25 min)
Pain Assessment and Management (73 min)
Patient Restraint and Seclusion (20 min)
UConn Health Stroke Program (10 min)
Clinical Learning Environment
Mistreatment in the Clinical Learning Environment (13 min)
Sleep Loss and Fatigue (25 min)
Medical School Requirements
ADA Acknowledgement (2 min)
Medical School Requirement Attestations (20 min)
Receipt of Policies and Procedures (2 min)
Residents as Teachers and Supervisors of Medical Students (Anesthesiology,
Dermatology, Emergency Medicine, Family Medicine, Internal Medicine, Neurology,
Neurosurgery, Primary Care, OBGYN, Pediatrics, Physical Medicine and
Rehabilitation, Psychiatry, Surgery) (20 min)
Diversity, Equity and Inclusion
GME Orientation (in person):
Diversity Training (60 min)
Vulnerable Populations Training (30 min)
Fall Courses for new interns / first year fellows:
Care Delivery, Culturally Competent (8 min)
Managing Patient Bias (12 min)
Microaggressions in Healthcare (20 min)
Supporting Gender Identity (10 min)
Welcoming Environment for LGBTQI (30 min)
Annual Courses – These courses must be done every year. These courses are also automatically assigned
in Healthstream in October and are due in December. (Note: If you complete these courses as an incoming
resident or fellow, you will not have to complete them again until your second year of training).
Approximately 4 hours to complete all courses.
Compliance/Regulatory
COVID 19 General Information on Infection Control (20 min)
Office of Healthcare Compliance & Privacy Training and IT Security (45 min)
Informed Consent (30 min)
OR Fire Safety/ Electrosurgery & The (Anesthesiology, Neurosurgery, OBGYN, Orthopedics, Hand
Surgery, Pediatric Orthopedics, Orthopedic Spine Surgery, Orthopedics Sports Medicine,
Otolaryngology, Surgery, Surgical Critical Care, Pediatric Surgery, Vascular Surgery, Maternal Fetal
Medicine, Reproductive Endocrinology, Acute Care, Pediatric Anesthesiology, Minimally Invasive
Gynecologic Surgery)
Managing Patient Bias (12 min)
Safe and Effective Process to Prepare Items for Sterilization (Emergency Medicine, Family Medicine,
Interventional Cardiology JDH, Pulmonary Critical Care, OBGYN, Orthopedics Sports Medicine,
Otolaryngology, Neonatology, Radiology, Surgery, Urology, Maternal Fetal Medicine, Reproductive

40
Residents/Fellows Policies and Procedures Manual
Endocrinology, Minimally Invasive Gynecologic Surgery, Emergency Medicine - International
Disaster)
Standard Precautions: Bloodborne Pathogens and Other Potentially Infectious Materials (50 min)
Workplace Violence
Patient Care
Abuse and Neglect: Identification, Assessment and Response (15 min)
Interpreter Services at UConn Health (15 min)
Clinical Learning Environment
Annual Residents as Educators Attestation (Anesthesiology, Dermatology, Emergency Medicine,
Family Medicine, Internal Medicine, Neurology, Neurosurgery, Primary Care, OB/GYN, Pediatrics,
Physical Medicine and Rehabilitation, Psychiatry, Radiology, Surgery) (1 min)
Sleep Loss and Fatigue (25 min)
Revised 11/17, 11/20, 3/21, 10/21, 12/21, 1/22, 2/22, 3/22. 4/22, 6/22, 9/22, 10/22, 3/23, 6/23, 3/24
Reviewed, 4/19, 2/20

41
Residents/Fellows Policies and Procedures Manual
EMERGENCY LIFE SUPPORT TRAINING
Basic Life Support certification is required of all residents/fellows at the University of Connecticut.
According to the ACGME and RC requirements for each program and in collaboration with the institutions
in which the residents/fellows are educated, it will be determined which levels and types of required
certification in life support skills will be acquired and maintained by resident/fellow participants. These
requirements will be made known to the residents/fellows by their respective programs.
Reviewed 3/15, 4/19, 3/21, 2/23
42
Residents/Fellows Policies and Procedures Manual
OCCUPATIONAL IONIZING RADIATION EXPOSURE
The Accreditation Council for Graduate Medical Education (ACGME) mandates that sponsoring institutions
assure a safe working environment for their residents/fellows. The purpose of this policy is to outline the
responsibilities and the mechanism for tracking resident/fellow radiation exposures from UConn Health
activities in addition to affiliated institutional sources of ionizing radiation.
1. The Residency and Fellowship Program Directors, in consultation with the Radiation Safety Officers at
each site, shall determine which residents/fellows may be subject to occupational exposure of ionizing
radiation and for whom personal radiation dosimetry is required.
2. All incoming residents/fellows will be provided an orientation on radiation safety, including a more
detailed orientation for those residents/fellows who are determined to require dosimetry monitoring
as determined in section 1.
3. All residents and fellows determined to be required to wear personal radiation dosimetry per section
1 will follow the UConn Health policy, Personal Radiation Dosimetry (policy Number 11-025) and the
procedure for personal dosimetry as outlined in the Procedures for Residents and Fellows Provided
Personal Radiation Dosimetry.
4. Residents/fellows are required to do a reading of their radiation safety badge(s) each between the 1
st
and 7
th
day of each month. Failure to comply with this monthly reading may impact your ability to
participate in clinical responsibilities until the reading is completed.
5. Residents/fellows are responsible for their assigned badge(s). If a badge is lost, the resident/fellow will
be responsible to pay the $32 lost badge charge
6. Pregnant residents/fellows need to read the UConn Health Declaration of Pregnancy Policy.
Residents/fellows who have questions or problems with their badge should direct questions to Versant
by emailing [email protected] with a “CC” to the GME Office GMEoffice@uchc.edu. The
GME Office will be monitoring questions and problems regarding badges.
Revised: 4/19, 10/19, 3/21, 2/23

43
Residents/Fellows Policies and Procedures Manual
REAPPOINTMENTS PROCESS AND REQUIREMENTS
The Graduate Medical Education (GME) Office is responsible for issuing all letters of initial
appointment/contracts as well as letters of reappointment/contracts for residents/fellows in the
University of Connecticut School of Medicine (UConn SOM) sponsored programs.
The primary responsibility for defining the standards of academic performance and personal and
professional development rests with the Program Director. The GME Office designee reviews
reappointment requirements for each resident/fellow. If all requirements have been met, a reappointment
letter/contract will be issued. The resident/fellow is responsible for reviewing, signing, and returning
his/her reappointment letter/contract to the GME Office.
A resident/fellow will receive a reappointment letter/contract prior to completion of the
resident’s/fellow’s current year of training. Therefore, the reappointment letter/contract is conditional
upon a resident/fellow meeting all requirements for promotion as defined by the resident’s/fellow’s
program.
A resident/fellow that has not met the requirements to be reappointed must be given written notice by
their program director that his/her reappointment/contract may not be renewed.
Documents required for a reappointment letter/contract to be issued by the GME Office include:
Reappointment request from the Program Director indicating good standing of a resident/fellow
Passing score transcript on the USMLE 3/COMLEX 3, if applicable
Documentation required before starting the next academic year:
Valid employment status
Completion of the annual Institutional Curriculum courses
Revised 4/17, 3/21, 2/23
Reviewed 4/19
44
Residents/Fellows Policies and Procedures Manual
REAPPOINTMENT LETTER/CONTRACT
Date: Program:
Name: Post Graduate Year Level:
Duration of Appointment:
Current Salary at this Level:
I understand that this appointment is contingent upon fulfilling all training requirements necessary to
advance to the next level and that this appointment must be returned within 14 days or my position as
described above may not be held. I also understand that I may be required to cover additional shifts,
beyond what is required as part of my program’s back-up or jeopardy policy (for which there is no
additional compensation), and if I cover additional shifts I will receive additional compensation
proportionate to the number of shifts covered up to $30,000.
By signing and returning this agreement, I agree to complete the full term of appointment as designated
above. I also agree to continue to abide by the terms, conditions and policies pertaining to my employment
and training in the above-named program as described in my initial letter of appointment. This includes,
but is not limited to policies on evaluation, promotion, due process, leave, and delinquent charts. I
understand that the Residents/Fellows Policies and Procedures Manual is updated regularly, and I am
responsible for complying with the current policies, procedures, etc.
We are pleased that you are continuing your training with us.
Sincerely,
Steven Angus, MD, FACP
Designated Institutional Official
I accept the offer to continue my training in the above program at the University of Connecticut School of
Medicine and employment with the Capital Area Health Consortium. I agree to abide by the terms and
conditions as described above and the more detailed description on the Residents/Fellows Policies and
Procedures Manual available at http://gme.uchc.edu.
_____________________________________________________ _______________________
Name Date
Reviewed 4/19, 2/21, 3/21

45
Residents/Fellows Policies and Procedures Manual
TRAINING AND EMPLOYMENT VERIFICATION
When a resident/fellow applies for a license or credentials for privileges in a hospital after
residency/fellowship, the GME Office will process any verification and malpractice claims history requests.
Requests/release of information forms can be faxed to 860-679-4624 or emailed to [email protected].
Reviewed 4/19, 2/21, 3/21, 2/23

46
Residents/Fellows Policies and Procedures Manual
USMLE 3/COMLEX 3
All PGY 1 residents must take USMLE 3/COMLEX 3 before the end of the PGY1 year. Residents who fail to
meet this requirement may not be permitted to participate in the training program beyond the end date of
their PGY 1 year contract. The program director, in consultation with the GME Office, will determine the
status of the resident with regards to the training program. Possible outcomes include but are not limited
to a required unpaid personal leave (benefits continued) of no longer than 3 months duration during which
time the resident must take USMLE 3/COMLEX 3 or non-renewal of contract.
If a resident enters a University of Connecticut School of Medicine residency program as a PGY 2 and has
not taken and passed USMLE 3/COMLEX 3, the resident must take USMLE 3/COMLEX 3 within the first 6
months of the PGY 2 year. The resident must pass USMLE 3/COMLEX 3 by the end of the PGY2 year.
Successful completion of USMLE 3/COMLEX 3 is a requirement to be promoted or appointed to the PGY 3
or above training level. Residents who fail to meet this requirement will not be permitted to participate in
the training program beyond the end date of their PGY 2 year contract. The program director, in
consultation with the GME Office, will determine the status of the resident with regards to the training
program. Possible outcomes include but are not limited to a required unpaid personal leave (benefits
continued) of no longer than 3 months duration during which time the resident achieves a passing score
or non-renewal of contract.
Residents seeking to enter a University of Connecticut School of Medicine residency program as a PGY 3 or
higher must have taken and passed USMLE 3/COMLEX 3. Fellows seeking to enter a University of
Connecticut School of Medicine fellowship program must have taken and passed USMLE 3/COMLEX 3.
Fellows who fail to meet this requirement will not be permitted to participate in the training program. The
program director, in consultation with the GME Office will determine the status of the fellow with regards
to the training program. Possible outcomes include but are not limited to delay of the fellow’s start date
until a passing score is provided or cancellation of the fellow’s appointment to the training program in
consultation with the National Residency Matching Program (NRMP).
Taking any leave (especially when multiple leaves or absences occur in the same contract year) may extend
the time necessary to complete the program requirements for graduation as well as for Board eligibility
(see Contract Extension Due to Leave Guidelines Policy). Residents/Fellows are responsible for
understanding their Residency Review Committee/Program requirements for program completion as well
as their Board requirements regarding Board eligibility, specifically as it relates to time away from their
program.
Revised 4/17, 1/20, 4/22
Reviewed 4/19, 2/21, 3/21, 2/23

47
Residents/Fellows Policies and Procedures Manual
GRADUATION/SEPARATION REQUIREMENTS
To graduate from a residency/fellowship program at the University of Connecticut School of Medicine, a
resident/fellow must:
have passed USMLE Step 3, COMLEX Step 3 or equivalent and provide proper documentation
have been evaluated as competent in all six ACGME competencies and milestones (if applicable) for
their program
have completed the required Institutional Curriculum
complete an exit survey conducted by the Capital Area Health Consortium
meet with the Program Director or designee to sign the Final Residency/Fellowship Training
Summary Verification form
complete all program exit requirements
attend an exit interview and complete the sign-out sheet with the Capital Area Health Consortium.
Exception: a resident/fellow who changes programs does not need to attend the exit interview or
complete the sign-out sheet until the completion of his/her last program at the University of
Connecticut School of Medicine.
If a resident/fellow leaves a residency/fellowship prior to successful completion of the program
requirements, only the last 3 items above must be completed.
All access to computer systems, including email, will be removed at the end of their last day of work.
Revised 2/16, 5/17, 2/23
Reviewed 4/19, 3/21

48
Residents/Fellows Policies and Procedures Manual
SALARY
The salary level is paid commensurate with the responsibility of the position. All residents/fellows in the
same program level are paid the same salary level. CAHC will pay the resident/fellow’s salary and fringe
benefits and will make the necessary federal, state, and employee benefit cost withholdings from the
resident/fellow’s bi-weekly payroll.
It is the responsibility of the resident/fellow to notify the CAHC and the Program Coordinator of address
changes while employed and upon leaving the program. CAHC is not responsible for lost or misplaced W-
2 forms (mailed in January), paychecks, or other mail.
Determination of tax-filing information is the responsibility of the resident/fellow. CAHC staff are not
authorized to advise residents/fellows on tax matters.
Revised 4/16, 5/17, 4/19, 1/23
Reviewed 3/21

49
Residents/Fellows Policies and Procedures Manual
BENEFITS
PROFESSIONAL LIABILITY/MALPRACTICE INSURANCE AND ADVERSE
EVENTS/INCIDENTS
Liability coverage is provided for residents/fellows only while they are carrying out assigned duties as part
of their residency/fellowship program for acts and omissions that are not wanton, reckless, or malicious.
Coverage includes claims filed after completion of the program for activity that occurred during their
program tenure. State law requires liability coverage to be provided by the hospital site where the
resident/fellow is working, with state indemnity covering all other approved assignments.
Since you enjoy what is probably the best medical malpractice protection available, generally you are
immune from personal civil suit and liability and indemnified from personal expense for activities
undertaken within the scope of your duties pursuant to C.G.S Sec. 4-141, full cooperation is also expected
once you have finished the residency program because suits may get filed after you have completed the
program. This cooperation is expected even if you are simply a fact witness and not the primary target of
the lawsuit. You will not have to pay for legal representation as this is part of the malpractice protection
afforded to you for acting withing the scope of your duties pursuant to C.G.S Sec. 4-141. Similarly your
cooperation is expected without charging the State in the defense of claims once you have left our
program.
A Professional Liability Letter is sent to hospitals, other Graduate Medical Education programs, and
licensing agencies when they inquire about malpractice coverage for the residents/fellows in University of
Connecticut School of Medicine sponsored programs. If claims history information is requested, Risk
Managers from all affiliated hospitals (and for any approved assignments outside one of the affiliated
hospitals or John Dempsey Hospital) are contacted to facilitate the process. If only general coverage
information is requested, a Professional Liability Letter is to be used.
Residents/fellows concerned about an adverse patient occurrence or circumstance (hereinafter “adverse
incident”) should contact the Program Director and Risk Management Office staff as soon as possible at the
site where the adverse incident occurred.
If a resident/fellow receives a subpoena or is contacted by a Risk Management Officer, an attorney, the
Connecticut Department of Health, or another investigating body regarding an adverse incident, the
resident/fellow should decline to discuss the matter until they can contact their Program Director and Risk
Management Office staff at the site of the adverse incident. Such contact should be made as soon as possible
following notification, particularly because prompt action may sometimes be required. A subpoena, for
example, constitutes a legal document that could require either a resident/fellow’s appearance to testify
under oath and/or the timely production of certain documents. The Program Director and Risk
Management Office at the site of the adverse incident will be familiar with the proper legal and other
procedures for such situations and will employ the appropriate escalation procedures depending upon the
specific circumstances.
The following procedures must be followed if you receive a subpoena or are contacted about an adverse
incident:

50
Residents/Fellows Policies and Procedures Manual
1. Contact your Program Director and Risk Management Office at the site of the adverse incident.
2. The Program Director will inform the institution’s Assistant Dean for Education of the
investigation. If the site does not have an Assistant Dean for Education, the Medical Director and
relevant Department Chair for the site will be contacted.
3. The Program Director will contact the UConn Graduate Medical Education Office designee.
4. The Program Director or designee and Risk Manager at the site will discuss with the
resident/fellow the nature of the investigation and what is expected from the resident/fellow
regarding the investigation.
5. The Program Director or designee and the Risk Manager will assist the resident/fellow in
determining whether the resident/fellow may benefit from a separate advocate throughout the
investigation.
“UConn Health and The UConn School of Medicine reserve the absolute discretion to provide independent
legal counsel to any resident/fellow involved in an adverse incident wherein the provision of such
independent counsel is deemed to be in the best interest of the physician and/or the State of CT/ UConn
Health/UConn School of Medicine and Dentistry.”
Professional activities outside the program are not covered under UConn’s liability coverage and are the
sole responsibility of the resident/fellow.
Revised 4/17, 4/19, 11/23
Reviewed 3/21, 2/23

51
Residents/Fellows Policies and Procedures Manual
LONG-TERM DISABILITY
All residents/fellows are provided a long-term disability (LTD) group policy issued by the Guardian Life
Insurance Company (GLIC). GLIC determines if a resident/fellow is eligible to receive benefits under the
policy when a claim is filed.
During the residency/fellowship training program, the LTD group policy is paid for by CAHC. For illnesses
that extend past 90 days, the LTD benefit will be $3,500 per month (taxable) for the approved disabled
period.
Residents/fellows actively working and not on an active leave of absence, may purchase Guaranteed
Standard Issue (GSI) coverage through GLIC at their own expense from the CAHC disability representatives
at any time while in training and up to 90 days post termination. If interested in GSI coverage, it is
recommended you reach out to CAHC’s disability representatives prior to applying for coverage with other
carriers. If you are rated or denied coverage with another carrier, you will become ineligible for the GSI
coverage. CAHC will review this benefit conversion with all residents/fellows at their exit meetings.
Additional or alternative disability options are available through the AMA and ACP. Consulting with an
insurance advisor or financial planner can provide valuable guidance in choosing the right coverage.
Any questions regarding the GLIC LTD coverage must be directed to CAHC. It is critical and required that
the resident/fellow also notify their Program Director as soon as it is known that the resident/fellow needs
a medical leave of absence regardless of the status of the receipt of LTD benefits.
Eligibility for workers compensation benefits may adversely affect eligibility for LTD. The CAHC can
provide information related to long-term disability benefits.
Revised 3/17, 4/17, 5/17, 4/19, 12/21, 1/23, 3/23, 6/24
Reviewed 3/21
52
Residents/Fellows Policies and Procedures Manual
WORK-RELATED INJURIES
Residents/fellows employed by the CAHC are covered for workplace injuries. A purple card will be
provided to all residents to outline the instructions on what to do if injured during their employment. This
card must be worn with the resident’s/fellow’s badge and shown upon seeking treatment at the teaching
facility where the injury occurred. A resident/fellow should not provide their health insurance card or
allow the treating facility to bill the resident/fellow personally. There are instructions for the providers/
facility on the purple card to direct each facility on billing procedures specific to their facility.
The program covers any work-related injury or illness arising out of and in the course of employment that
requires medical, surgical, or hospital treatment. No matter how minor an on-the-job injury may appear, it
is important that a resident/fellow immediately report any on-the-job injury to their supervisor, as set
forth below and a First Report of Injury must be completed. Failure to report an incident promptly may
result in the denial of workers’ compensation benefits or a delay. All absences due to a work-related injury
or workers’ compensation claim count towards a Family and Medical Leave of Absence (FMLA) if the
resident/fellow is eligible for FMLA (see Family and Medical Leave of Absence).
Neither the CAHC nor its insurance carrier will be liable for the payment of workers' compensation benefits
for injuries that occur during a resident’s/fellow’s voluntary participation in any off-duty recreational,
social, or athletic activity sponsored by the CAHC.
It is the resident's/fellow’s responsibility to
Notify their supervisor and CAHC of an accident or injury occurring while on the job and help
complete a First Report of Injury
Keep their supervisor and CAHC informed of their medical status related to any work-related injury
or workers’ compensation claim on an on-going basis
Follow the authorized treating physician’s treatment plan
Keep medical appointments and avoid any activity which will further aggravate the injury or illness
Accident or Injury information
During the day, the resident/fellow must go to the site’s Employee Health Department whenever
possible.
Off-hours the resident/fellow should go to the Emergency Department of the working site.
• If at Connecticut Children’s Medical Center (Connecticut Children’s), go to Hartford Hospital’s
Employee Health Department. If after hours, go to Hartford Hospital’s Emergency Department.
If there is a medical emergency and no emergency department at the site where the injury
occurred, go to UConn’s Employee Health or Emergency Department depending on the time of day.
If necessary, go to the nearest hospital’s emergency department.
The incident must be reported by the resident/fellow to the CAHC within 24 hours of the injury. If
off-hours, leave a message with the date, time, place, and nature of the injury and the
resident’s/fellow’s contact number.
53
Residents/Fellows Policies and Procedures Manual
The site where the injury/illness occurred will be responsible for completing a Work-Related
Injury/Illness form and sending it to the CAHC as soon as possible. This site will also maintain medical
records related to the injury and perform necessary follow-up visits. If a resident/fellow wishes to go to
any outside provider in the State of Connecticut, the Employee Health Department or CAHC can provide a
form that will allow direct billing to CAHC for the services provided. If the worker’s compensation carrier
denies the claim as a work-related injury, the expenses may be covered through the group health plan if
expenses are remitted within 90 days of the injury.
Taking any leave (especially when multiple leaves or absences occur in the same contract year) may
negatively impact time necessary to complete the program requirements for graduation as well as for
Board eligibility (see Contract Extension Due to Leave Guidelines). Any work-related injury or workers’
compensation leave that goes beyond 12 weeks may result in the termination of the appointment with
UConn SOM and the end of employment with CAHC. Residents/fellows are responsible for understanding
their Residency Review Committee/program requirements for program completion as well as their Board
requirements regarding Board eligibility, specifically as it relates to time away from their program.
Revised 6/16, 3/17, 5/17, 1/23, 6/24
Reviewed 4/19, 3/21

54
Residents/Fellows Policies and Procedures Manual
SALARY ADVANCE AND ORIENTATION PAY
Residents/fellows receive an annual salary based on their current PGY level. Housestaff required to attend
GME and program orientation prior to their June start date will receive additional compensation of $1,500.
Please note the first paycheck, including orientation pay, can only be received once residents/fellows have
met all onboarding requirements to begin training.
A salary advance of up to $2,000 (no interest) is available to any new incoming resident/fellow upon arrival
to the area. This advance bridges the gap between orientation and receipt of their first paycheck. This is a
limited program for incoming residents/fellows only and excludes those not required to orient in advance
of their contract start date. A minimum of $200 per pay period will be deducted from the
resident's/fellow’s paycheck beginning in August until the salary advance is paid back.
Please contact the residency/fellowship program coordinator to initiate the process for an advance.
DEPENDENT CARE REIMBURSEMENT ACCOUNT
Capital Area Health Consortium (CAHC) employees may qualify for a pre-tax dependent care
reimbursement account. Qualified employment-related dependent care expenses are those expenses
incurred so that residents/fellows can be gainfully employed. Monies will be deducted from payroll on a
pre-tax basis and reimbursed post-tax upon submission of qualified expense invoices. Residents/fellows
may contribute up to $5,000 annually; unused funds are forfeited per IRS code if not used within the
calendar year.
MEDICAL, DENTAL, AND VISION INSURANCE
Medical, dental, and vision insurance is provided for all residents/fellows employed by the Capital Area
Health Consortium (CAHC) at a low cost and is deducted pre-tax from the bi-weekly payroll. Coverage for
all J-1 exchange visitors and accompanying J-2 dependents will be in accordance with the U.S. Code of
Federal Regulations (22 CFR 62.14). There is a pre-tax payroll deduction per paycheck to cover employee,
spouse and/or children. For academic year starts, coverage begins on the first full day of employment. For
off-cycle starts dates, coverage is effective on the date of hire. The insurance covers hospitalization,
medical-surgical, major medical, prescription drug, dental, and vision (if elected).
The CAHC staff must be made aware of any changes in dependent status within 30 days of the event (i.e.,
marriage, birth, divorce). When a change occurs, please contact the CAHC staff for a new application.
LIFE INSURANCE
Group term life insurance is provided at no cost to all full-time residents/fellows employed by the Capital
Area Health Consortium (CAHC). The effective date is the first day of employment. The basic benefit is one
time the annual salary, up to $50,000. For accidental death and dismemberment, the benefit is three times
the annual salary, up to $150,000. Each resident/fellow must fill out and sign a beneficiary form included
in each onboarding packet. If a resident/fellow elects not to take the insurance or not select a beneficiary,
a waiver form must be completed.

55
Residents/Fellows Policies and Procedures Manual
A resident/fellow must notify CAHC when changes in beneficiary are necessary. A change of beneficiary
form is available on the website https://health.uconn.edu/graduate-medical-education/cahc/benefits-
and-payroll/.
A copy of the group insurance certificate is available on the CAHC website.
TAX-SHELTERED INVESTMENT PROGRAM
Capital Area Health Consortium (CAHC) has a Tax-Sheltered (403b) Investment Plan for its employees. The
plan offers numerous funds and fund managers to select investment options. The account can be easily
transferred to another qualified plan or an individual retirement account upon program completion.
Monies may be deducted from each paycheck on a pre-tax basis (403B) and/or a post-tax basis (Roth). The
pre-tax option reduces the amount of income taxed increasing net pay. The funds become taxable upon
distribution at retirement. For the Roth post-tax option, taxes are withheld, and the earnings and
contributions are not taxable upon distribution at retirement (please see IRS rules for further clarification).
This is a voluntary benefit, and there are no matching employer contributions. CAHC is responsible
only for the payroll deduction and remitting the contribution to the investment institution. CAHC is
not responsible for any investment decisions.
COBRA INSURANCE COVERAGE CONTINUATION
When a resident/fellow ends their employment, they may extend their current health insurance by electing
COBRA coverage and paying the monthly premium to CAHC. Spouses and children covered by the group
health plan also have the right to choose continuation coverage.
The continuation coverage may be purchased monthly for up to 18 months and can be cancelled at any
time.
A Consortium staff member will meet with each exiting resident/fellow to provide the COBRA paperwork
and explain the details. In the event of a resident/fellow divorce or death, COBRA may be purchased
monthly for up to 36 months by the spouse.
Revised 4/17, 12/21, 1/23, 6/24
Reviewed 4/19, 3/21
LOAN DEFERMENTS
Residents/fellows with undergraduate loans are usually eligible for some form of loan deferment. The GME
Office staff will verify residency/fellowship status and will keep copies of all forms sent in the GME Office.
Residents/fellows should contact their loan institution for forms.
Reviewed 4/19, 3/21, 2/23

56
Residents/Fellows Policies and Procedures Manual
EDUCATIONAL RESOURCE ALLOWANCE
Residents and fellows are provided an educational resource allowance (“ERA”) during
residency/fellowship. ERA can be used on items such as books, journal subscriptions, online educational
materials, USMLE Step 3, surgical loupes, stethoscopes, laptops, tablets, and smart phones. ERA may also
be used to support scholarship at educational venues as a supplement to the financial support outlined in
the Educational Travel section of this policy book. Items purchased with ERA must be used for the
purpose of furthering the resident/fellow’s education as it relates to their training program.
Residents/fellows in the below programs are provided with the following financial support for their ERA;
1 year preliminary program (PGY 1) * $500
1 year preliminary program (PGY 2) ** $1,000
3 year residency program $2,500
4 year residency program w/o prelim at UConn *** $3,000
4 year residency program w/ prelim at UConn *** $3,500
5 year residency program w/o prelim at UConn **** $4,000
5 year residency program w/ prelim at UConn **** $4,500
7 year residency program $6,500
1 year fellowship program $1,000
2 year fellowship program $2,000
3 year fellowship program $3,000
Amounts are calculated based on PGY 1= $500, PGY 2-7 = $1,000 per year. Any exceptions to the standard
accredited program length may result in pro-rating the above amount or adjusting the calculation as
applicable.
ERA is not appropriated for added research year(s). ERA is not appropriated for grant funded programs.
The following rules must be adhered to by the resident/fellow to qualify for reimbursement:
Receipts must be submitted to the GME Office within 6 months of the date of purchase. Please
note that graduating residents must make purchases by and submit a request for reimbursement
no later than April 1st of the graduating year.
Residents/fellows should not pay for items until they receive pre-approval from their program
coordinator via email or other formal correspondence. In the event that a resident or fellow has
paid for an item and pre-approval was not granted, the resident or fellow will not be reimbursed.
The resident/fellow must purchase the item themselves and must provide proof of this. Purchases
made on behalf of a resident/fellow by an outside person will not be reimbursed. Comparable
purchases (i.e., multiple tablets, computers, phones) made within 12 months of each other must be
accompanied by a written justification for the second purchase.
Purchases or portions of purchases made with gift cards, store credit, or reward points are not
reimbursable.
Any submitted reimbursements to the program/ GME office deemed an “abuse of funds” will
result in the forfeiture of the amount in question. Program discipline may follow as appropriate.

57
Residents/Fellows Policies and Procedures Manual
Examples of “abuse of funds” are as follows but not limited to using ERA for gifts, altering receipt
amounts, and altering names on receipts.
The GME Finance Manager will provide final oversight/approval regarding the appropriate use of the
Educational Resource Allowance.
* = medicine/surgery prelim year; ** = surgery non-categorical position; *** = anesthesiology, dermatology, neurology;
**** = radiology
Revised 4/17, 3/21, 6/24
Reviewed 4/19, 2/23
58
Residents/Fellows Policies and Procedures Manual
EDUCATIONAL TRAVEL
Residents and fellows in good standing are provided financial support to attend an educational conference
pertinent to their specialty. All travel (including virtual) to educational conferences must be approved by
the resident/fellow’s Program Director. Residency/fellowship programs may have a listing of conferences
that are appropriate for residents/fellows to attend. Residents/fellows should refer to their individual
program manuals for further information.
Once approved by the resident/fellow’s Program Director, final approval is required by the Director of
GME Finance.
Residents and fellows should not pay for conference registration, transportation or accommodations until
they receive final approval. In the event that a resident or fellow has paid for educational conference
registration, transportation or accommodations and final approval is not granted, the resident or fellow
will not be reimbursed. Receipts must be submitted within 6 months of return from approved travel.
Failure to do so may result in denied reimbursement.
All components of travel must be executed in the most cost efficient means possible. Ground versus air
travel, choice of airfare, and lodging must be in accordance with UConn policy as displayed at:
https://health.uconn.edu/finance/travel/policies-and-procedures/ (air & ground)
https://health.uconn.edu/finance/travel/lodging/ (lodging)
The financial support available to attend an educational conference is as follows:
Interns/Residents: Up to $2,000 will be supported during residency for PGY1-5 and an additional
$2,000 for PGY6-7 from the training program’s budget.
Fellows: Up to $2,000 will be supported per year from the training program’s budget.
Additional funding up to a maximum of $2,000 during residency/fellowship may be approved if a
resident/fellow is presenting UConn GME related research as the primary author at an educational
conference (in-person or virtual). Such funding also requires approval by the resident/fellow’s Program
Director and the Director of GME Finance as outlined above. This additional funding is not available for a
resident/fellow presenting research at a conference done outside of the scope of their UConn
residency/fellowship program (i.e.: in medical school).
International educational conference travel will be considered for financial support on a case by case basis.
Such funding also requires approval by the resident/fellow’s Program Director and the Director of GME
Finance as outlined above.
Revised 3/15, 11/17, 1/20, 3/21
Reviewed 3/17, 4/19

59
Residents/Fellows Policies and Procedures Manual
SECTION II: COMPLIANCE AND INTEGRITY
60
Residents/Fellows Policies and Procedures Manual
CONFLICT OF INTEREST/ VENDOR INTERACTIONS
Purpose of Policy
The purpose of this policy is to establish policy for interactions with pharmaceutical, nutraceutical,
Biotech, Device, Hospital, Research Equipment, and Supplies Industries
(Biomedical) industry
representatives for residents/fellows of the University of Connecticut
School of Medicine (UConn SOM).
Interactions with Industry representatives occur in a variety of contexts, including marketing of new
products, educational support of residents/fellows, and continuing medical education (CME).
Residents/fellows also participate in interactions with Industry representatives off campus and in
scholarly publications. Many aspects of these interactions are positive and important for promoting
the
educational, clinical and research missions of UConn SOM. However, these interactions must be ethical
and cannot create conflicts or perceived conflicts of interest that could endanger patient safety,
data
integrity, the integrity of the education or the reputation of UConn SOM and the
affiliated sites.
Residents/fellows must be aware of the National Physician Payment Transparency Program (Open
Payments). This program aims to increase public awareness of financial relationships between industry
and health care providers. The intent of Open Payments is to create a national resource for
beneficiaries, consumers and providers to know more about the relationships among physicians,
teaching hospitals and industry by requiring industry to report to CMS any payments or other transfers
of value they make to physicians and teaching hospitals. Medical residents/fellows are currently
excluded from the definition of physicians for the purposes of the Open Payments program. Further
details can be found at the Center for Medicare and Medicaid services
(https://www.cms.gov/OpenPayments).
Statement of Policy
It is the policy of UConn SOM Graduate Medical Education (GME) Program that interactions with the
Industry should be conducted so as to avoid or minimize conflicts of interest. When conflicts of interest
do arise, they must be addressed appropriately, as described
below.
Scope of Policy
This policy covers interactions between residents/fellows and Industry during working
hours. The
policy incorporates the following types of interactions:
I. Gifts and compensation
II. Site access by sales and marketing representatives
III. Provision of scholarships and other educational funds to residents/fellows
IV. Support for educational and other professional activities
V. Acceptance of free medication, supplements, device, and other product samples
VI. Disclosure of relationships with Industry
VII. Training of residents/fellows regarding potential conflict of interest in interactions with
Industry
VIII. References
I. Gifts and Compensation
A. Personal gifts from Industry may not be accepted by residents/fellows at any clinical
facility in which GME occurs. This includes UConn SOM affiliated sites.

61
Residents/Fellows Policies and Procedures Manual
1. No form of personal gift from Industry can be accepted by residents/fellows
2. Unrestricted educational grants may be provided by industry to the Program
Director or
designee on behalf of the program but not directly to residents/fellows or teaching
faculty. Unrestricted educational grants are funds given to a program
for future
educational activities (i.e., to bring a speaker or visiting professor for
teaching rounds or
conferences; purchase of teaching materials or books; or pay for
an off-site educational
meeting). The program maintains full control of how the
funds are used. Credit can be
given to the funding Industry/ies that have donated
the unrestricted educational grant.
3. Educational materials such as textbooks may be provided by Industry to the Program
Director or designee on behalf of the program at the Program Director’s discretion.
Identifying labels such as pharmaceutical inserts or logos must be removed or covered
prior to their use with residents/fellows.
4. Medical staff at non-UConn-operated clinical facilities may accept gifts but may not
provide these to residents/fellows without prior review by
the Program Director or
designee.
B. Residents/fellows may not accept gifts or compensation for listening to a sales talk by an
Industry representative.
C. Residents/fellows may not accept gifts or compensation for prescribing or changing a
patient's prescription, food supplement, or device.
D. Residents/fellows must consciously and actively divorce clinical care decisions from any
perceived or actual benefits expected from any company.
E. Residents/fellows may not accept direct compensation, including the defraying of costs,
for
attending a Continuing Medical Education (CME) or other activity or conference,
unless the
resident/fellow is speaking or otherwise actively participating at the event.
II. Graduate Medical Education Site Access by Sales and Marketing Representatives
A. Sales and marketing representatives are not permitted in any direct patient care areas in
which GME occurs and where protected health information is accessible, with one
exception: when providing necessary training on a previously purchased device or a device
considered for purchase, and in the presence of teaching faculty. This training
must adhere
to HIPAA privacy rules.
B. Sales and marketing representatives are permitted in non-patient care areas of graduate
medical education, by appointment only, with faculty or with faculty and residents/fellows,
in the setting of faculty supervision of trainee-industry interactions.
III. Provision of Scholarships and Other Educational Funds to Residents/Fellows
A. Industry support of residents/fellows must be free of any actual or perceived conflict of
interest, must be specifically for the purpose of education, and must comply with all of the
following:
1. UConn SOM Program Director or designee selects the resident/fellow.
2. The funds are provided to the program and not directly to the resident/fellow.
3. The Program Director or designee has determined that the funded conference or
program has educational merit.
4. The resident/fellow is not subject to any implicit or explicit expectation of providing
something in return for the support, i.e., a "quid pro quo."
62
Residents/Fellows Policies and Procedures Manual
B. This provision may not apply to national or regional merit-based awards, which will be
reviewed by the Program Director on a case-by-case basis.
IV. Support for Educational and Other Professional Activities
A. Programs must be aware of the Accreditation Council for Continuing Medical Education
(ACCME) Standards for Commercial Support. They provide useful guidelines for
evaluating all forms of Industry interaction, both on and off campus and including
UConn-sponsored and other events. The Standards may be found at www.accme.org.
B. All education events sponsored by UConn SOM programs must be compliant with ACCME
Standards for Commercial Support whether or not CME credit is awarded.
1. Educational grants that are compliant with the ACCME Standards may be received
from
Industry by the program. ACCME guidelines include:
a. Financial support by Industry is fully disclosed by the meeting sponsor.
b. The meeting or lecture content is determined by the speaker and not the
Industrial sponsor.
c. The lecturer is expected to provide a fair and balanced assessment of therapeutic
options and to promote objective scientific and educational activities and
discourse.
d. UConn SOM resident/fellow or teaching faculty participant is not required by
an Industry sponsor to accept advice or services concerning speakers, content,
etc.,
as a condition of the sponsor's contribution of funds or services.
C. Meals or other types of food directly funded by Industry may not be provided for
Residents/fellows. Unrestricted educational funds may be provided to a Program
Director
or designee on behalf of the program and expended for refreshments at
resident/fellow
educational sessions. The contributing Industry/ies can be credited for
contributing an
unrestricted educational grant for the session.
D. This provision does not apply to meetings of professional societies that may receive
partial
Industry support or professional meetings governed by ACCME Standards.
V. Acceptance of Free Samples
A. Teaching faculty may accept free drug, nutraceutical, or device samples from industry for
distribution to patients by residents/fellows. This acceptance must occur in administrative
(non-patient care) areas.
B. Since distribution of sample products to patients may encourage use of costlier products,
residents/fellows and teaching faculty should be cautious in distributing such products.
C. Free samples may never be sold.
D. Free samples should not be used by residents/fellows or teaching faculty for themselves
or
family.
VI. Disclosure of Relationships with Industry
A. Residents/fellows are prohibited from publishing articles under their own names that
are written in whole or material part by Industry employees.
B. In scholarly publications, residents/fellows must disclose their related financial interests
in accordance with the International Committee of Medical Journal Editors
(http://www.icmje.org).
63
Residents/Fellows Policies and Procedures Manual
VII. References
AMA Statement on Gifts to Physicians from Industry (https://www.ama-
assn.org/delivering-care/ethics/gifts-physicians-industry ).
The Accrediting Council for Continuing Medical Education Standards for Commercial
Support (www.accme.org).
Reviewed 3/14, 5/17, 4/19, 3/21, 2/23
64
Residents/Fellows Policies and Procedures Manual
HIPAA/PRIVACY AND SECURITY OF CONFIDENTIAL DATA
CONFIDENTIAL DATA
The University of Connecticut School of Medicine (UConn SOM) and affiliated sites have policies and
procedures governing the privacy and security of confidential data (including but not limited to patient’s
personal health information). These policies also establish requirements for the security and appropriately
controlled release of all such information, consistent with applicable federal and state laws, including the
federal privacy rule. Residents and fellows must abide by the policies and procedures governing privacy
and security of confidential data at the University of Connecticut School of Medicine (UConn SOM) as well
as at all affiliated sites.
Confidential data includes, but is not limited to, personally identifiable information that is not in the public
domain and if improperly disclosed could be used to steal an individual’s identity, violate the individual’s
right to privacy or otherwise harm the individual and/or the institution. (see UConn Health’s
Confidentiality Policy.)
In the course of the resident’s/fellow’s employment, the resident/fellow may be granted access to various
types of Confidential data, including but not limited to:
• Patient information that is protected by both Connecticut and federal laws, such as the Health
Insurance Portability Accountability Act (“HIPAA”).
• Sensitive UConn Health information not in the public domain
• Financial information (budgets, strategic revenue plans, accounts receivable/payable details)
• IDs and/or Passwords for access to UConn Health computing resources
• Research data requiring protections
Security of confidential data is governed by policy on the acceptable use of electronic resources (see UConn
Health’s Acceptable Use Policy)
PATIENT INFORMATION
Confidential patient information includes (but is not limited to) any information about health status,
provision of health care, or payment for health care that is created or received by a resident/fellow, another
medical professional, or a health care institution, and can be linked to a specific individual. This includes
patient information in written, oral or electronic form.
Residents/fellows shall not access or disclose confidential patient information except as may be required
by law and the applicable policies or procedures of any site in which the resident/fellow may train.
Residents/fellows have a responsibility to keep secure and confidential the information collected about
patients during their encounters with healthcare professionals. Releasing parts or all of that information
is appropriate under certain circumstances, such as when treating the patient, providing for continuity of
care, participating in approved research and educational activities, complying with laws, and assuring
reimbursement for services provided
65
Residents/Fellows Policies and Procedures Manual
UConn Health has specifically developed a policy to guide residents/fellows in the use of patient data for
educational purposes. (see The Use of PHI in Education policy)
UConn Health’s Privacy and Security Policies linked here provide guidance to residents/fellows to assure
patient rights are protected:
https://health.uconn.edu/policies/policies-specific-areas/specific-area-hipaa-security/
Revised 4/16, 5/17, 9/17, 11/17, 4/19, 3/21
Reviewed 2/23

66
Residents/Fellows Policies and Procedures Manual
ACCESSING MEDICAL RECORDS
Residents/fellows should only access medical records through the electronic medical record system (i.e.:
EPIC) for work related purposes.
Residents/fellows who wish to view their own medical records must do so through the patient portal
(i.e.: MyChart) and not via the electronic medical record system.
Residents/fellows who need to view the medical records of a family, friend or coworker may only do so if
granted proxy access to the records through the patient portal and not via the electronic medical record
system.
Created 3/21
67
Residents/Fellows Policies and Procedures Manual
PROHIBITION OF DISCRIMINATION AND DISCRIMINATORY HARASSMENT,
INCLUDING SEXUAL HARASSMENT AND SEXUAL ASSAULT, INTIMATE PARTNER
VIOLENCE, AND STALKING
The University of Connecticut (the “University”) is committed to maintaining a safe and non-discriminatory
learning, living and working environment for all members of the University community – students,
employees, residents, fellows, patients and visitors. Academic and professional excellence can exist only
when each member of our community is assured an atmosphere of safety and mutual respect. All members
of the University community are responsible for the maintenance of an environment in which people are
free to learn and work without fear of discrimination, discriminatory harassment or interpersonal
violence. Discrimination diminishes individual dignity and impedes equal employment and educational
opportunities.
The University does not unlawfully discriminate in any of its education or employment programs and
activities on the basis of an individual’s race, color, ethnicity, religious creed, age, sex, marital status,
national origin, ancestry, sexual orientation, genetic information, physical or mental disability (including
learning disabilities, intellectual disabilities, and past or present history of mental illness), veteran’s status,
prior conviction of a crime, workplace hazards to the reproductive system, gender identity or expression,
or membership in any other protected classes as set forth in state or federal law. To that end, UConn’s
Policy Against Discrimination, Harassment and Related Interpersonal Violence, Including Sexual and
Gender-Based Harassment, Sexual Assault, Sexual Exploitation, Intimate Partner Violence, Stalking,
Complicity, Retaliation and Inappropriate Amorous Relationships (the “Policy”) prohibits specific forms of
behavior that violate state and federal laws, including but not limited to Title VII of the Civil Rights Act of
1964 (“Title VII”), Title IX of the Education Amendments of 1972 (“Title IX”), the Violence Against Women
Reauthorization Act of 2013 (“VAWA”), and related state and federal anti-discrimination laws. Such
behavior may also require the University to fulfill certain reporting obligations under the Jeanne Clery
Disclosure of Campus Security Policy and Campus Crime Statistics Act (the “Clery Act”), as amended by
VAWA, and Connecticut state law regarding reporting suspected child abuse and neglect.
The University prohibits discrimination, as well as discriminatory harassment, sexual assault, sexual
exploitation, intimate partner violence, stalking, sexual or gender-based harassment, complicity in the
commission of any act prohibited by UConn Policy, retaliation against a person for the good faith reporting
of any of these forms of conduct or participation in any investigation or proceeding under UConn Policy
(collectively, “Prohibited Conduct”). These forms of Prohibited Conduct are unlawful and undermine the
mission and values of our academic community. In addition, inappropriate amorous relationships with
employees in positions of authority can undermine the University’s mission when those in positions of
authority abuse or appear to abuse their authority. See Section 3E for more information on amorous
relationships prohibitions.
UConn’s Policy Against Discrimination, Harassment and Related Interpersonal Violence articulates the
University’s commitment to: (1) eliminating, preventing, and addressing the effects of Prohibited Conduct;
(2) fostering a safe and respectful University community; (3) cultivating a climate where all individuals are
well-informed and supported in reporting Prohibited Conduct; (4) providing a fair and impartial process
for all parties in the investigation and resolution of such reports; and (5) identifying the standards by which
violations of this Policy will be evaluated and disciplinary action may be imposed. In addition, the
68
Residents/Fellows Policies and Procedures Manual
University conducts ongoing prevention, awareness, and training programs for employees and students to
facilitate the goals of this Policy.
A student or employee determined by the University to have committed an act of Prohibited Conduct is
subject to disciplinary action, up to and including separation from the University. Third Parties who
commit acts of Prohibited Conduct may have their relationships with the University terminated and/or
their privileges of being on University premises withdrawn.
It is the responsibility of every member of the University community to foster an environment free of
Prohibited Conduct. All members of the University community are encouraged to take reasonable and
prudent actions to prevent or stop an act of Prohibited Conduct. The University will support and assist
community members who take such actions.
Retaliation against any individual who, in good faith, reports or participates in the reporting, investigation,
or adjudication of Prohibited Conduct is strictly forbidden.
For more information, individuals may contact:
The Office of Institutional Equity & Title IX Coordinator
UConn Health
16 Munson Road, 4th Floor
Farmington, CT 06030
Mail Code MC 5310
(860) 679-3563
equity@uconn.edu
www.equity.uconn.edu
www.titleix.uconn.edu
www.accessibility.uconn.edu
Revised 2/16, 5/17, 8/17, 4/19
Reviewed 3/21, 2/23
69
Residents/Fellows Policies and Procedures Manual
FACULTY, STAFF, AND STUDENT RELATIONS
The relationships between faculty, staff, residents, fellows and patients should demonstrate the highest
standards of ethical conduct in all educational settings and be conducted without abuse, humiliation,
harassment and exploitation of relationships for personal gain or advantage. Any questions, concerns or
breaches in professional relations may result in disciplinary action and should be brought immediately to
the attention of the Designated Institutional Official (DIO)/designee. Possible ramifications of violations in
standards of ethical conduct include review and subsequent disciplinary action which could ultimately lead
to termination/dismissal.
In particular, all faculty and staff, including residents and fellows, must be aware that amorous
relationships with students are likely to lead to difficulties and have the potential to place faculty and staff
at great personal and professional risk. The power difference inherent in the faculty-student or staff-
student relationship means that any amorous relationship between a faculty or staff member and a student
is potentially exploitative or could at any time be perceived as exploitative and should be avoided. In the
event of a charge of Sexual Harassment arising from such circumstances, the University will in general be
unsympathetic to a defense based upon consent when the facts establish that a faculty-student or staff-
student power differential existed within the relationship.
Moreover, amorous relationships between supervisors and their subordinate employees often adversely
affect decisions, distort judgment, and undermine workplace morale for all employees, including those not
directly engaged in the relationship. Any University employee who participates in supervisory or
administrative decisions concerning an employee with whom s/he has or has had an amorous relationship
has a conflict of interest in those situations.
Accordingly, the University prohibits all faculty and staff from pursuing or engaging in amorous
relationships with undergraduate students; prohibits all faculty and staff from pursuing or engaging in
relationships with graduate students under that faculty or staff member’s authority; and prohibits all
faculty and staff from pursuing or engaging in amorous relationships with employees whom they
supervise.
UConn’s Policy Against Discrimination, Harassment and Related Interpersonal Violence, Including Sexual
and Gender Based Harassment, Sexual Assault, Sexual Exploitation, Intimate Partner Violence, Stalking,
Complicity, Retaliation and Inappropriate Amorous Relationships sets forth the University’s conduct
expectations regarding amorous relationships in greater detail.
Revised 8/17, 4/19
Reviewed 3/21, 2/23

70
Residents/Fellows Policies and Procedures Manual
SOCIAL NETWORKING
Social and business networking websites (i.e., Instagram, LinkedIn, Facebook, Twitter, Flickr, etc.) and cell
phone texting are increasingly being used for communication by individuals as well as businesses and
universities. As such, it has become necessary to outline appropriate individual and University of
Connecticut School of Medicine (UConn SOM) Graduate Medical Education (GME) sanctioned use.
Guiding Principles
Privacy and confidentiality between physician and patient is of the utmost importance.
Respect among colleagues and co-workers must occur in a multidisciplinary environment.
The tone and content of all electronic communication must remain professional.
The individual is responsible for the content of his/her own blogs/posts/texts.
Material published on the web should be considered permanent.
Any information posted on the Internet is public information.
Texts may be intercepted and should not be considered secure communication unless using any
approved system provided by UConn GME. Such as, TigerConnect, Voalte, etc.
All health care providers have an obligation to maintain the privacy of patient health information as
outlined by the Health Insurance Portability and Accountability Act (HIPAA).
Residents/fellows should adhere to all principles outlined in the Residents/Fellows Policies and
Procedures Manual and Code of Conduct for Residents/fellows when interacting on the internet.
Internet use and texting must not interfere with the timely completion of job duties.
Personal blogging or posting of updates should not be done during work hours or with work
computers.
It is always inappropriate to “friend” or “follow” patients on any social networking site or to check
patient profiles.
Texting about and posting of any sensitive, proprietary, confidential, private and PHI or financial
information about UConn SOM or any affiliated site is prohibited. See Policy: Confidentiality UCHC
policy #2002-43.
Obtaining cell phone photographs or videos of any patient is prohibited except as allowed in Policy:
Visual, Audio or Recording of Patient Data Obtained Through Any Medium, UCHC policy #2014-03
(Visual, Audio or Recording of Patient Data Obtained Through Any Medium).
Refrain from posting or texting any material that is obscene, defamatory, profane, libelous,
threatening, harassing, abusive, hateful or embarrassing to another person or any other entity. This
includes, but is not limited to, comments regarding UConn Health or any other affiliated hospitals
or employees of them.
Any personal legal liability imposed for any published content will be the responsibility of the
resident/fellow. Texts are discoverable even if deleted from the cell phone.
Social networking sites and texting can be the source of cyber bullying, harassment, stalking, threats
or unwanted activity. Contact the UConn Health Police Department or the Graduate Medical
Education Hotline for assistance.
Patient Information
71
Residents/Fellows Policies and Procedures Manual
Identifiable protected health information (PHI) should NEVER be published on the Internet. This
applies even if only the patient is able to identify themselves from the posted information.
Residents/fellows must adhere to HIPAA principles at all times.
Communication Regarding UConn SOM or affiliated sites
Unauthorized use of UConn SOM information or logos is prohibited. No phone numbers, email
addresses, web addresses, name of the department or UConn SOM may be posted without permission
from an authorized departmental individual. For identification purposes, a resident/fellow may list the
affiliation with the UConn SOM.
In all communication where a resident/fellow is listed as being affiliated with the UConn SOM or a
department of UConn, a disclaimer must be attached such as: “All opinions and views expressed, in my
profile (on my page) are entirely personal and do not necessarily represent the opinions or views of
anyone else, including other faculty, staff, residents/fellows or students in my department at UConn.
Neither my department nor UConn have approved the material contained in this profile (on this page).
I take sole responsibility for this content.”
Offering Medical Advice
It is never appropriate to provide medical advice on a social networking site.
Privacy Settings
Residents/fellows should consider setting privacy at the highest level on all social networking sites.
Disciplinary Action
Resident/fellow discipline follows the Code of Conduct Violations/Non-Academic Review Procedures
Policy. Disciplinary action will be determined by the Program Director and will vary depending on the
nature of the policy violation.
Revised 4/16, 5/17, 4/19
Reviewed 3/21, 2/23
72
Residents/Fellows Policies and Procedures Manual
DRUG-FREE WORKPLACE ACT
UConn Health prohibits students, residents/fellows and employees from the unlawful manufacture,
distribution, dispensing, possession, or use of alcohol, drugs, or other controlled substances in its facilities,
during UConn Health-sponsored activities, and while employees are on the job or subject to duty.
Residents and fellows, while not paid employees of UConn Health, must abide by UConn Health policies
and procedures while engaged in a UConn Health-sponsored residency/fellowship program.
Residents/fellows therefore must abide by UConn Health’s policy Drug-Free Schools & School Campuses
Ac and Drug-Free Workplace Act.
Any resident/fellow who violates this policy may be disciplined, up to and including termination.
Counseling and support services are available to any resident/fellow with alcohol or drug-related
problems (see Counseling Services).
Reviewed 4/19, 3/21, 2/23

73
Residents/Fellows Policies and Procedures Manual
PROFESSIONAL ATTIRE/DRESS CODE
Residents/fellows are expected to be professionally dressed, well-groomed and must maintain a
professional demeanor. It is very important to promote an appropriate view of the institution, build patient
trust and maintain a safe work environment. Appearance should conform to the standards/norms of the
clinical and nonclinical setting in which the resident/fellow is working.
This policy outlines minimum standards. Programs and affiliated sites may have more stringent
requirements which should be followed.
Supervisors have the right to determine compliance with this policy. A resident/fellow that is deemed
inappropriately dressed may be sent home and corrective action may be taken.
Identification
The ID badge and coat (if applicable) for the hospital currently training in should be worn and clearly
visible for all clinical encounters. Badges should be worn above the waist.
If an ID badge is lost or stolen, the police department of the appropriate hospital should be contacted
as soon as possible to report the loss and to make arrangements for replacement.
ID badges are the property of the hospital and must be returned upon termination of training and
employment.
Footwear
All employees must wear shoes that are appropriate to their job. Shoes should be clean and in good
repair. Closed-toed shoes are required in patient care areas and areas where extra protection may be
needed (research labs). In addition, OSHA requires that protective clothing/covering be worn that will
prevent blood or other potentially infectious materials from reaching the skin.
Flip-flops, slippers, open toed shoes, and excessively high-heeled shoes are examples of inappropriate
footwear.
Clothing
Clothing should fit properly, be clean and in good condition. Business casual is appropriate for most
areas. Do not wear clothing that is non-professional in appearance, length, or fit such as:
Any clothing including lab coats that are soiled or torn
Shorts, skorts, miniskirts shorter than above the knee or deeply slit skirts
Cut offs, overalls, leather pants, legging, stretch pants or sweatpants
Bare shoulders, midriff or backs (tank or tube tops, halter tops, spaghetti straps or strapless tops or
dresses)

74
Residents/Fellows Policies and Procedures Manual
Any attire that is considered provocative or exposing undergarments (too tight, low cut, below the
waist or sheer clothing)
Scrubs should only be worn in the operating room (pre and post as well) unless indicated by the
program’s dress code.
Grooming and Hygiene Standards
Good personal hygiene and cleanliness is an essential part of providing high-quality service. Patients,
guests and staff have a right to expect general cleanliness and good oral hygiene. Hair should be worn
to prevent contamination or cause a safety hazard. Facial hair should be neatly trimmed and
maintained. Some things to avoid:
Fragranced lotion, perfume or cologne
Smoke odors
Artificial nails, extenders and embedded jewelry
Revised 2/16, 5/17, 4/19, 2/23
Reviewed 3/21

75
Residents/Fellows Policies and Procedures Manual
DELINQUENT MEDICAL RECORD PROCEDURE
The timely completion of medical records is important to safe and effective patient care. All clinical learning
environments have requirements regarding medical records completion.
When a resident/fellow fails to complete required patient records within the time limit determined by the
relevant clinical service and/or hospital, they can be removed from clinical service and educational
responsibilities until those records are complete. Residents/fellows may be required to make up time
away from clinical service and educational responsibilities which may result in an extension of training.
Revised 3/15, 5/17, 4/19
Reviewed 3/21

76
Residents/Fellows Policies and Procedures Manual
SECTION III: PROFESSIONAL ACTIVITIES
AND PROFESSIONALISM

77
Residents/Fellows Policies and Procedures Manual
RESIDENT/FELLOW JOB DESCRIPTION
Organizational Relationships
The University of Connecticut School of Medicine appoints a resident or fellow (collectively referred to as
the trainees or individually as trainee) physician, to a graduate medical education residency or fellowship
training program for the length of the enrolled training program.
Faculty members at the University of Connecticut, and other participating sites, provide supervision to the
trainee.
Position Overview
The position of trainee involves a combination of supervised, progressively more complex and
independent patient evaluation and/or management functions, formal educational, and research activities.
Provision of healthcare and other professional services provided by the trainee is commensurate with the
trainee’s level of advancement and competence, under the general supervision of appropriately privileged
attending teaching faculty. Trainees must meet program requirements specific to their discipline as well
as board eligibility requirements in order to successfully complete training.
Responsibilities
The trainee is both a learner and a member of the healthcare team. Responsibilities (essential job
functions) of a trainee that must be achieved with or without reasonable accommodations include:
• Satisfactory progress in training program as measured by program goals and objectives and
milestones as applicable
• Meeting Technical Performance Standards
• Participation in safe, effective and compassionate healthcare
• Participation in institutional orientation, the educational activities of the training program, and
other required education programs within the institution or at a participating site/sites
• Assumption of responsibility for teaching and supervising other trainees and students and
participation in other activities involving the clinical staff, as appropriate
• Participation in institutional committees and councils to which the trainee is appointed or invited
• Maintenance of certification (ACLS, PALS, ATLS, etc.) as required by enrolled training program
• Maintenance of the appropriate permitting or licensure, where necessary, while appointed by the
University of Connecticut to a training program
• Documentation of cases and procedures, where appropriate, as directed by the enrolled training
program and mandated accreditation body
• Performance of duties in accordance with the established practices, procedures, and policies of
training programs, the University of Connecticut, clinical departments, and other participating
institutions to which the trainee is assigned
• Recognition of personal conditions or situations which may affect patient safety or progress in
training, and communication of this to program leadership

78
Residents/Fellows Policies and Procedures Manual
• Compliance with University of Connecticut policies and enrolled training program clinical and work
hour requirements which include:
o Work within typical business hours, beyond typical business hours, unpredictable hours, or a
combination of all
o Work up to 80 hours per week, averaged over a four-week period, inclusive of all in-house call,
clinical and educational activities, and clinical work done from home
o Work multiple consecutive days including weekends with a minimum of one day in seven, free
from all educational and clinical responsibilities, averaged over a four-week period, inclusive of
call
o Return to work after eight hours off between scheduled clinical work and education periods
o Work a maximum of 24 hours of continuous duty in the hospital followed by up to an additional
4 hours on-site for patient safety, education, and effective transitions of care
o Assignment of in-house call as often as every third night (when averaged over a four-week
period)
o Limit program-approved extra credit and/or moonlighting activities to comply with clinical and
work hours requirements and extra credit and/or moonlighting policies
Qualifications (Eligibility Criteria)
The physician trainee must meet eligibility requirements of the University of Connecticut School of
Medicine for participation in a residency or fellowship program.
All trainees must provide proof of the legal right to work as required by federal law.
Technical Performance Standards
Trainees must demonstrate the ability to meet the following technical performance standards which are
an integral part of the Trainee (Resident and Fellow) Job Description.
Patient Care and Procedural Skills
• Provide healthcare under the supervision of faculty; the faculty member with direct responsibility
for the trainee has the authority to decide which activities the trainee will be allowed to perform
within the context of the assigned levels of responsibility
• Gain competence and progressive autonomy, progressing from on-site and contemporaneous
supervision to more indirect and periodic supervision as training progresses
• Understand and interpret complex healthcare information
• Synthesize information acquired in person and via remote technology
• Interpret causal connections and make accurate, fact-based conclusions based on available data and
information
• Formulate a hypothesis, investigate the potential answers and outcomes, and reach appropriate and
accurate conclusions
• Identify emergency situations and respond in a timely manner

79
Residents/Fellows Policies and Procedures Manual
• Meet applicable safety standards for the environment and follow universal precaution procedures
Medical Knowledge
• Learn through a variety of modalities, including, but not limited to, providing healthcare under the
supervision of faculty, didactic instruction, simulation and other laboratory instruction, physical
demonstrations, team and collaborative activities, individual study, preparation and presentation
of reports, and use of technology
Practice Based Learning & Improvement
• Demonstrate capacity for self-reflection and life-long learning
• Set learning and improvement goals
• Demonstrate progress on educational milestones
• Incorporate formative feedback into daily practice
Interpersonal and Communication Skills
• Demonstrate effective communication, participation, and collaboration in person and in writing
• Perceive, appropriately interpret, and respond to another’s emotional state, including verbal and
non- verbal communication
• Communicate publicly, including teaching and group presentations
Professionalism
• Demonstrate independent prioritization of conflicting or simultaneous demands
• Perform or direct complex, varied or multiple tasks simultaneously
• Maintain confidentiality of information
• Work effectively within multidisciplinary teams
• Exercise good judgment
• Complete all responsibilities in a timely manner
• Adapt to changing environments and function in the face of uncertainties inherent in healthcare
• Demonstrate compassion, integrity, and concern for others
• Work with colleagues and provide healthcare for all individuals in a respectful and effective manner
regardless of gender identity, age, race, sexual orientation, religion, disability, or any other
protected status
• Understand, and function within, the legal and ethical aspects of professional practice
• Display ethical and moral behaviors commensurate with the role of a professional in all interactions
with patients, faculty, staff, trainees, and the public
Systems-based Practice
• Learn and comprehend processes and procedures

80
Residents/Fellows Policies and Procedures Manual
• Recognize safety hazards in the clinical environment, e.g., infection risk, needle sticks, agitated
patient etc., and follow standard processes and procedures to mitigate risk
Definitions:
Technical performance standards are those duties and responsibilities that the individual must be able
to perform with or without a reasonable accommodation.
Residency is the phase of formal medical education beginning at graduation from medical school and
ending after the educational requirements for the specialty certifying board has been completed.
Fellowship is additional training in a subspecialty after completing residency or graduate training.
Work hours are all clinical and academic activities related to the program; i.e., patient care (both inpatient
and outpatient), administrative duties relative to patient care, the provision for transfer of patient care;
time spent on in-house clinical and education activities, clinical work done from home, and scheduled
activities, such as conferences. Work hours do not include reading and preparation time spent away from
the work site.
Created 4/21

81
Residents/Fellows Policies and Procedures Manual
PROFESSIONALISM
The Graduate Medical Education Training Programs of the University of Connecticut School of Medicine
are committed to the highest standards of professionalism to all persons, agencies and associations. This
foremost includes our patients, their families and other visitors. We believe that professionalism and the
image we present inspires confidence in the care and services we provide as professionals and as an
institution.
We expect that trainees must demonstrate a commitment to carrying out professional responsibilities and
an adherence to ethical principles, including:
• compassion, integrity, and respect for others;
• responsiveness to patient needs that supersedes self-interest;
• respect for patient privacy and autonomy;
• accountability to patients, society and the profession; and,
• sensitivity and responsiveness to a diverse patient population, including but not limited to
diversity in gender, age, culture, race, religion, disabilities, and sexual orientation;
• a safe, comfortable and healthy work environment;
• presenting a professional and identifiable appearance to patients, their families and visitors,
UConn Health staff, and the medical and business communities; and
• supporting a culture of confidence and service excellence while at the same time,
accommodating sincerely held religious and cultural beliefs when operationally feasible.
Reviewed 4/19, 3/21
82
Residents/Fellows Policies and Procedures Manual
COMPACT BETWEEN TRAINEES AND THEIR TEACHERS
(Trainees include medical students, residents, and fellows)
(Adopted from the AAMC Compact)
Medical education is an integral component of the formal education of physicians. In order to practice
medicine independently, physicians must receive a medical degree and successfully complete a supervised
period of residency/fellowship training in a specialty/subspecialty area. To meet their educational goals,
trainees must participate actively in the care of patients and must assume progressively more
responsibility for that care as they advance through their training. In supervising trainees, faculty must
ensure that trainees acquire the knowledge and special skills of their respective disciplines while adhering
to the highest standards of quality and safety in the delivery of patient care services. In addition, faculty
members are charged with nurturing those values and behaviors that strengthen the doctor-patient
relationship and that sustain the profession of medicine as an ethical pursuit.
Core Tenets of Medical Education
Excellence in Medical Education
Institutional medical education leadership and program faculty must be committed to maintaining high
standards of educational quality. Trainees are first and foremost learners. Accordingly, a trainee’s
educational needs should be the primary determinant of any assigned patient care services. The
learning objectives of the program should not be compromised by excessive reliance on trainees to
fulfill non-physician service obligations. (Trainees however, must remain mindful of their oath and
recognize that their responsibilities to their patients always take priority as the primary part of their
educational considerations.)
Highest Quality Patient Care and Safety
Preparing future physicians to meet patients’ expectations for optimal care requires that they learn in
clinical settings epitomizing the highest standards of medical practice. Indeed, the primary obligation
of institutions and individuals providing medical education is the provision of high quality, safe patient
care. Program faculty must ensure that trainees are integrated and actively participate in
interdisciplinary clinical quality improvement and patient safety programs. By allowing trainees to
participate in the care of their patients, faculty accepts an obligation to ensure high quality medical care
in all learning environments.
Respect for Trainee Well-Being
Fundamental to the ethic of medicine is respect for every individual. Trainees are especially vulnerable,
and their well-being must be accorded the highest priority. Given the uncommon stresses inherent in
fulfilling the demands of their training program, trainees must be allowed sufficient opportunities to
meet personal and family obligations, to pursue a balance of work and life activities, and to obtain
adequate rest.
Commitments of Faculty
1. As role models for our trainees, we will maintain the highest standards of care, respect the needs
and expectations of patients, and embrace the contributions of all members of the healthcare team.

83
Residents/Fellows Policies and Procedures Manual
2. We pledge our utmost effort to ensure that all components of the educational program for trainees
are of high quality, including our own contributions as teachers.
3. In fulfilling our responsibility to nurture both the intellectual and the personal development of
trainees, we commit to fostering academic excellence, exemplary professionalism, cultural
sensitivity, and a commitment to maintaining competence through life-long learning.
4. We will demonstrate respect for all trainees, without regard to gender, race, national origin,
religion, disability or sexual orientation; and we will cultivate a culture of tolerance among the
entire staff.
5. We will do our utmost to ensure that trainees have opportunities to participate in patient care
activities of sufficient variety and with sufficient frequency to achieve the competencies required
by their chosen discipline. We also will do our utmost to ensure that trainees are not assigned
excessive clinical responsibilities and are not overburdened with services of little or no educational
value. The learning objectives of the educational program will be accomplished through an
appropriate blend of supervised patient care responsibilities, clinical teaching, and didactic
educational events and will not be compromised by excessive reliance on trainees to fulfill non-
physician service obligations.
6. In fulfilling the essential responsibility we have to our patients, we will ensure that trainees receive
appropriate supervision for all of the care they provide during their training. In the clinical learning
environment, each patient will have an identifiable, appropriately credentialed and privileged
attending physician who is ultimately responsible for that patient’s care. We will provide trainees
with opportunities to exercise graded, progressive responsibility for the care of patients, so that
they can learn how to practice medicine and recognize when, and under what circumstances, they
should seek assistance from colleagues. Faculty members functioning as supervising physicians will
delegate portions of care to trainees based on the needs of the patient and the skills of the trainee.
7. We will do our utmost to prepare trainees to function effectively as members of healthcare teams.
We will provide an environment that maximizes effective communication and the opportunity for
trainees to work as members of effective inter-professional teams that are appropriate to the
delivery of patient care.
8. We will evaluate each trainee’s performance on a regular basis, provide appropriate verbal and
written feedback, and document achievement of the competencies required to meet all educational
objectives.
9. We will ensure that trainees have opportunities to partake in required conferences, seminars and
other non-patient care learning experiences and that they have sufficient time to pursue the
independent, self-directed learning essential for acquiring the knowledge, skills, attitudes, and
behaviors required for entering residency and subsequent independent practice.
10. We will ensure a culture of patient safety and professionalism by educating our faculty members
and our trainees’ concerning the personal responsibility of physicians to appear for duty
appropriately rested and fit so that they may provide the services required by their patients.
Commitments of Trainees
1. We acknowledge our fundamental obligation is to place our patients’ welfare uppermost; quality
health care and patient safety will always be our prime objectives.
2. We pledge our utmost effort to acquire the knowledge, clinical skills, attitudes and behaviors
required to fulfill all objectives of the educational program and to achieve the competencies deemed
appropriate for our chosen discipline.

84
Residents/Fellows Policies and Procedures Manual
3. We embrace the professional values of honesty, compassion, integrity, and dependability.
4. We will adhere to the highest standards of the medical profession and pledge to conduct ourselves
accordingly in all of our interactions. We will demonstrate respect for all patients and members of
the health care team without regard to gender, race, national origin, religion, economic status,
disability or sexual orientation.
5. As trainees we learn most from being involved in the direct care of patients and from the guidance
of faculty and other members of the healthcare team. We understand the need for faculty to
supervise all of our interactions with patients.
6. We accept our obligation to secure direct assistance from faculty or appropriately experienced
residents/fellows whenever we are confronted with high-risk situations or with clinical decisions
that exceed our confidence or skill to handle alone.
7. We welcome candid and constructive feedback from faculty and all others who observe our
performance, recognizing that objective assessments are indispensable guides to improving our
skills as physicians.
8. We also will provide candid and constructive feedback on the performance of our fellow trainees,
and of faculty, recognizing our life-long obligation as physicians to participate in peer evaluation
and quality improvement.
9. We recognize the rapid pace of change in medical knowledge and the consequent need to prepare
ourselves to maintain our expertise and competency throughout our professional lifetimes.
10. In fulfilling our own obligations as professionals, we pledge to assist trainees in learning to meet
their professional obligations including but not limited to teaching providing feedback.
11. We will embrace a culture of patient safety and professionalism by understanding and accepting
our personal responsibility to appear for duty appropriately rested and fit so that we may provide
the care required by our patients.
We believe that the relationship between faculty and trainees should reflect the highest standards of ethical
conduct in all educational settings. Interactions between faculty and trainees must be conducted without
abuse, humiliation, harassment or exploitation of relationships for personal gain or advantage. Any trainee
or faculty member who experiences mistreatment or who bears witness to unprofessional behavior must
report such incidents according to the policies and procedures provided by the School of Medicine and the
Office of Graduate Medical Education (see Resident/Fellow Mistreatment).
This compact serves both as a pledge and as a reminder to trainees and their teachers that their conduct
in fulfilling their obligations to one another is the medium through which the profession perpetuates its
standards and inculcates its ethical values.
For more information about the Compact, go to http://www.aamc.org/residentcompact.
I agree to this Compact.
__________________________________________________________ ___________________
Name (print) and signature Date
Approved by Education Council: 2/12/06
Reviewed 3/08, 6/10, 3/14, 3/15, 4/17, 3/21, 2/23
Revised 9/11, 1/13, 11/17, 4/19

85
Residents/Fellows Policies and Procedures Manual
CODE OF CONDUCT
Residents/fellows should strive for excellence in all aspects of their personal and professional lives. This
implies a professional demeanor and conduct in direct patient care and in interactions with patients, family
members, other healthcare professionals, support staff and the public. It also implies an assurance of
integrity in both a resident’s/fellow’s professional and personal lives through behavior that is consistent
with establishing a level of trust and a professional reputation that are essential to the physician-patient
relationship and to the provision of high quality patient care.
The University of Connecticut School of Medicine (UConn SOM) and all of its major affiliates have codes of
conduct that apply to resident/fellow participation in program related duties wherein residents/fellows
are expected to act in a professional, courteous, respectful, and confidential manner. The resident/fellow
contract states that residents/fellows shall abide by all rules, regulations and bylaws of the program,
clinical department, and institution in which they are assigned. Violating these rules may be cause for
disciplinary action up to and including dismissal (see Code of Conduct Violations/Non-Academic
Deficiencies Review Procedures). Residents/fellows may be placed on Administrative Leave as appropriate
for investigation into an alleged Code of Conduct violation (see Administrative Leave ).
Conduct that is considered to be in violation of this code includes, but is not limited to, the following:
Unlawfully distributing, dispensing, selling or offering for sale, possessing, using or being under the
influence of alcohol, drugs, or a controlled substance when on the job, or in a position to be called into
work, subject to duty; or smelling of alcohol or having the odor of alcohol on the breath.
Misusing or willfully neglecting property, funds, materials, equipment or supplies from any of the
affiliate sites.
Fighting or acting in any manner that endangers the safety of oneself or others.
Destroying property in any way.
Stealing or possessing without authority any equipment, tools, materials, or other property of any of
the affiliated sites.
Refusing to do assigned work.
Academic misconduct such as cheating.
Research misconduct such as misrepresentation of activities.
Falsifying attendance records or hours worked.
Falsifying records.
Providing patient care under circumstances of physical, mental or emotional lack of fitness that could
interfere with the quality of care.
Being repeatedly or continuously absent or late, or being absent without notice or justifiable reason.
Conducting oneself in any manner which is offensive, intimidating, physically threatening, verbally
abusive or contrary to common decency or morality.
Carrying out any form of harassment, including sexual harassment.
Providing medical advice or information to patients without authorization.
Providing medical care outside of the scope of the resident/fellow permit. This includes writing
prescriptions for patients that are not under the resident’s/fellow’s direct care.
Providing non-emergent treatment to a person not under one’s care as part of the residency/fellowship
program (ex. family members or oneself).

86
Residents/Fellows Policies and Procedures Manual
Failing to comply with any of the major affiliates’ confidentiality policies and/or applicable
confidentiality laws.
Failing to report a police investigation or an arrest involving you to your Program Director.
Engaging in behavior which is below the professionalism standards of the residency/fellowship
program.
Engaging in activities that violate UConn SOM’s, any of the affiliate sites’ or the State of Connecticut’s
“Code of Ethics.”
Gambling or unauthorized solicitation in the workplace.
Work computer abuse, such as, but not limited to, accessing or viewing offensive or pornographic
material, misuse of computer accounts, unauthorized destruction of files, creating illegal accounts,
possession of or use of unauthorized password, disruptive or annoying behavior on the computer and
non-work-related utilization of computer software or hardware.
Being convicted of a crime.
Failure to cooperate or to be truthful in a program-related investigation.
If a Violation of the Code of Conduct has occurred, corrective disciplinary action may result (see Code of
Conduct Violations/Non-Academic Deficiencies Review Procedures).
Revised 3/15, 3/17, 4/19, 3/21
Reviewed 2/23
87
Residents/Fellows Policies and Procedures Manual
RESIDENTS, FELLOWS, and FACULTY WELL-BEING
The Office of Graduate Medical Education is committed to ensuring that residents/fellows remain
physically, mentally, emotionally, and spiritually healthy while participating in their training program.
Residency can be an inherently stressful time. Physicians are at increased risk for burnout and depression.
Self-care is an important component of professionalism and is a skill that must be learned.
The GME Office maintains a Well-Being website that provides information regarding resources aimed at
supporting and enhancing resident/fellow wellness (https://health.uconn.edu/graduate-medical-
education/wellness/).
The Office of Graduate Medical Education provides a mechanism for resident/fellow self-assessment of
burnout. While we will ask residents/fellows to complete this assessment twice yearly, the tool is always
available for self-administration. If a resident/fellow is in need of speaking to someone with a different
perspective, the Office of Graduate Medical Education offers FREE counseling services through the
Employee Assistance Program and FREE psychiatric care for individuals in need (see Counseling Services).
The Capital Area Health Consortium (CAHC) provides these services at no cost to the resident/fellow. There
is no need for a resident/fellow to notify his/her Program Director, the CAHC or their health insurance
carrier when accessing the Employee Assistance Program (EAP) and the Mental Health Services listed
below. A resident/fellow also may opt to utilize a provider of his/her choosing at their own expense and/or
through their health insurance carrier. Residents/fellows also have access to urgent or emergent care 24
hours a day, seven days a week through the emergency department at local hospitals.
Employee Assistance Program (EAP): All residents/fellows may contact the EAP at UConn Health to access
counseling services from psychologists, social workers, and marriage counselors. There is no limit to the
number of sessions provided.
http://health.uconn.edu/occupational-environmental/employee-assistance-program/
UConn Health Employee Assistance Program, 860-679-2877
Programs provide residents and fellows the opportunity to attend medical, mental health, and dental care
appointments, including those scheduled during their working hours.
The Graduate Medical Education Office encourages residents/fellows and faculty members to alert a
program director, the GME Office, and/or other personnel if there is ever a concern that another resident,
fellow, or faculty member may be displaying signs of burnout, depression, substance abuse, suicidal
ideation, or potential for violence.
If you or a colleague are in crisis, immediate help is available. Access care by calling 911, going to a
local emergency room, or by calling the National Suicide Prevention Lifeline (1-800-273-TALK
(8255)).
Revised 10/20, 8/22, 2/23; Reviewed 3/21

88
Residents/Fellows Policies and Procedures Manual
WORK ENVIRONMENT
The University of Connecticut School of Medicine will provide each resident/fellow with a work
environment that promotes the success of the resident/fellow in reaching the goals for their
educational program. The environment will comply with all the ACGME Institutional requirements and
Common Program Requirements, as well as the specific program requirements of the Residency Review
Committee for the program.
The Sponsoring Institution will ensure a healthy and safe clinical and educational environment that
provides for:
• access to food during clinical and educational assignments
• sleep/rest facilities that are safe, quiet, clean, and private, and that must be available and accessible
for residents/fellows, with proximity appropriate for safe patient care
• safe transportation options for residents/fellows who may be too fatigued to safely return home on
their own
• clean and private facilities for lactation with proximity appropriate for safe patient care, and clean
and safe
• refrigeration resources for the storage of breast milk
• safety and security measures appropriate to the clinical learning environment site
• accommodations for residents/fellows with disabilities, consistent with the Sponsoring
Institution’s policy
Program Requirements
The Program Directors and institutions shall ensure a culture of professionalism that supports
resident/fellow education, patient safety and personal responsibility.
The Program Directors shall ensure that residents/fellows are integrated and actively participate in
interdisciplinary clinical quality improvement and patient safety programs.
The programs and institutions shall minimize the number of transitions in care, and optimize the
effectiveness in transitioning care by designing, teaching and monitoring hand-over processes.
All programs will educate faculty and residents/fellows to recognize the signs of sleep deprivation and
fatigue and to manage fatigue mitigation processes. Programs and institutions will have processes in
place to manage the potentially negative effects of fatigue.
Programs will ensure that appropriate supervision is in place for all residents/fellows who care for
patients. The level of supervision for all activities at each level of training will be defined using the
classification provided in the common program requirements. The basis for progressive authority and
level of supervision will be defined and implemented by the program and its faculty.

89
Residents/Fellows Policies and Procedures Manual
Residents/fellows shall care for patients in an environment that maximizes effective communication.
This shall include the opportunity to work as a member of effective inter-professional teams that are
appropriate to the delivery of care in the specialty.
Programs shall ensure that resident/fellow compliance with all clinical and educational work hour
standards is monitored and achieved. Documentation of that compliance must be accomplished and
verified.
Revised 3/15, 5/17, 3/21, 2/23
Reviewed 4/19

90
Residents/Fellows Policies and Procedures Manual
CLINICAL AND EDUCATIONAL WORK HOURS RULES/PROCEDURES
The ACGME common program requirements allow for greater flexibility within an established framework
to provide programs and residents discretion to structure clinical experiences that best support
professional development. This added flexibility caries responsibilities for residents, who must recognize
when they are too fatigued to provide safe, high quality patient care and to programs and faculty who must
ensure that residents remain within the 80-hour maximum limit. The following institutional clinical and
educational work hour (duty hour) statement states the minimum requirements that each program
must follow. In addition, each program must have a written policy on resident/fellow clinical and
educational work (duty) hours. In developing of such policy, consideration should be given to the
educational opportunities for and personal well-being of the residents/fellows, and the needs of the
patient, including patient safety, and continuity of care. All policies must be in compliance with the policies,
procedures and requirements of the University of Connecticut School of Medicine (UConn SOM) and the
requirements of all relevant accrediting bodies (i.e., Accreditation Council for Graduate Medical Education
(ACGME) and Residency Review Committee (RRC)).
Clinical and educational work (duty) hours are defined as all required clinical and academic activities and
include patient care (inpatient and outpatient), all administrative duties related to patient care, in-house
call, moonlighting/extra-credit rotations, clinical work done from home, scheduled academic activities (i.e.,
conferences, morning report, lectures, etc.), and research that is a required part of the
residency/fellowship program. It does not include reading and preparation time spent away from the
University of Connecticut School of Medicine and its affiliated hospitals.
The requirements are as follows:
Clinical and educational work hours are limited to no more than 80 hours per week, averaged over a
4-week period inclusive of in-house call, clinical and educational activities, clinical work done from
home and all moonlighting/extra credit.
Programs that schedule residents to work 80 hours will likely violate the 80-hour rule, Therefore, in
order to maintain an emphasis on flexibility, programs should not schedule residents/fellows for more
than 75 hours per week averaged over 4 weeks in order to ensure all clinical and educational work
responsibilities can be met by the resident/fellow within the 80-hour limit
Residents/fellows must be provided with 1 day (defined as a continuous 24-hour period) in 7 free from
all clinical and academic activities, averaged over a 4-week period. At home call may not be assigned
on these free days.
Clinical and educational work periods for residents must not exceed 24 hours of continuous scheduled
clinical assignments. Up to four (4) hours of additional time may be used for activities related to patient
safety such as providing effective transitions of care and/or resident education. Additional patient care
responsibilities must not be assigned during this time.
Residents/fellows should have eight (8) hours off between scheduled clinical and educational work
periods. There may be instances when the resident chooses to stay to care for a patient or return to the
hospital with fewer than eight (8) hours free. This flexibility may be exercised within the context of the
80-hour and the one-day-off-in-seven requirements. Residents must have at least 14 hours free of
clinical work and education after 24-hours on in-house call.
91
Residents/Fellows Policies and Procedures Manual
Night float experiences must occur within the context of the 80-hour and one-day-off-in-seven
requirements.
In-house call must occur no more frequently than every third night, averaged over a 4-week period.
Program Directors must be notified if residents/fellows trade call schedules. Such trading should not
violate the every third night restriction.
PGY 1 residents are not allowed to take at-home call.
At-home call is not subject to the every-third-night limitation, but must not be so frequent or taxing as
to preclude rest or reasonable personal time. Time spent on patient care activities by residents on home
call must count towards the 80-hour maximum weekly limit. Residents/fellows taking at-home call
must have 1 day in 7 free from all clinical and academic responsibilities, averaged over a four-week
period.
Residents/fellows must have the written permission from the Program Director to participate in extra
credit rotations at any University of Connecticut affiliated hospital.
All extra credit rotations must be part of the program and therefore, count toward the duty hour limit.
If moonlighting is permitted by the program, the resident/fellow must get permission from the
Program Director to participate, and that all hours worked must be approved by the Program Director
and count towards the 80-hour work week (see Moonlighting/Extra Credit).
Residents/fellows are responsible for timely and honest completion of all clinical and educational
entries. Failure to enter hours honestly may result in a Code of Conduct violation.
All residency and fellowship programs must comply with UConn SOM’s duty hour restrictions as well as
any restrictions specified by their respective RC. Resident/fellow programs may not request an exemption
from these restrictions.
The Graduate Medical Education Committee (GMEC) is responsible for monitoring compliance with the
duty hour requirements. Recording of duty hours must be performed electronically in MyEvaluations.com
or another GME-approved electronic format.
There may be times when a program is participating in a national duty hour study where modifications to
the above may be in place.
Residents/fellows may report concerns about Clinical and Educational Work Hours through several
avenues.
See the Reporting Concerns Policy
Revised 4/19, 1/21
Reviewed 3/21, 2/23

92
Residents/Fellows Policies and Procedures Manual
FATIGUE MITIGATION
Residents/fellows are expected to come to work fit for duty. When a resident/fellow identifies themselves
or an attending identifies the resident/fellow as being too fatigued to drive home there are several options
for the resident/fellow:
Call rooms/sleep quarters are available at each hospital
A taxi or rideshare service (e.g. Uber, Lyft) can be utilized and will be reimbursed by the CAHC. The
resident/fellow will initially pay for the service. A receipt should be submitted to the program
coordinator for reimbursement. This service is available to take the resident/fellow to their home only.
The resident/fellow is responsible for securing his/her own transportation back to the hospital or
his/her vehicle.
Public (i.e., bus) or private (i.e., friend, spouse) transportation if available.
Annual training regarding fatigue mitigation is required of all residents/fellows. See Institutional
Curriculum.
Reviewed 3/15, 5/17, 4/19, 3/21, 2/23

93
Residents/Fellows Policies and Procedures Manual
TRANSITIONS OF CARE/HANDOVER
Purpose: The purpose of these guidelines is to establish standards within the UConn-sponsored Graduate
Medical Education programs to ensure that Transitions of Care and Handover occur in such a manner that
the quality and safety of patient care is not compromised.
The term “Transitions of Care” refers to the movement patients make between health care practitioners
and/or settings. Examples of Transitions of Care include:
• Admission to the hospital from an outpatient setting, including but not limited to the Emergency
Department, a medical office, a procedure center, or a diagnostic area such as the Radiology
Department.
• Admission of a patient to the hospital from another healthcare facility, including but not limited to
an outside hospital or skilled nursing facility.
• Transfer of a hospitalized patient to a different level of care within the hospital (i.e.: from the floor
to the stepdown unit or ICU or vice versa).
• Transfer of patient care responsibilities from one practitioner to another. This includes but is not
limited to the transfer of care that occurs: at the time of shift/duty hour changes for practitioners
(handover or “sign out”); at a time when a patient is transferred from one service to another; at a
time when a patient is to have a procedure or diagnostic study
• Discharge, including discharge to home or to another facility such as a skilled nursing facility or
rehabilitation facility
“Handover” refers to the transfer of information and of responsibility for patient care from one practitioner
to another. The Handover process must include, at a minimum, written communication from one provider
to the next. Verbal plus written communication is preferred as this allows for the opportunity for the
accepting provider to ask questions or to seek clarification when necessary.
The content of the information provided during the Handover process should include, at a minimum, the
following information in a standardized format that is universal across all services:
• Identification of patient: name, medical record number, and date of birth
• Location of patient (i.e.: hospital room number)
• Identification of responsible attending of record
• Diagnosis and current status/condition of patient
• Recent events, including changes in condition or treatment, current medication status, recent lab
tests
• Potential issues that may arise with anticipatory guidance where possible (Use “if/then” statements
whenever possible)
• List of tasks to complete with a plan and a rationale
• Allergies
• Code status

94
Residents/Fellows Policies and Procedures Manual
Standards: Individual training programs must adhere to institutional policies concerning transitions of
patient care. Each program must supplement these institutional Transition of Care/Handover guidelines
with requirements relevant to and specific for their specialty.
Individual training programs must design schedules and clinical assignments to maximize the learning
experience for residents while minimizing the number of Transitions of Care/Handovers for patients.
Programs are required to develop scheduling and Transitions of Care/Handover processes to ensure that:
• Residents do not exceed the 80 hour per week work hour limit averaged over 4 weeks.
• Faculty members are scheduled and available for appropriate supervision levels according to the
requirements for the scheduled residents.
• All parties involved in a particular program and/or Transition/Handover process have access to
one another’s schedules and contact information. All call schedules are available electronically.
• Patients are not inconvenienced or endangered in any way by frequent transitions in their care.
• All parties directly involved in the patient’s care before, during, and after the transition have
opportunity for communication, consultation, and clarification of information.
• Safeguards exist for coverage when unexpected changes in patient care may occur due to
circumstances such as resident illness, fatigue, and emergency.
Each program must include the Transition of Care/Handover process in its curriculum. Residents must be
directly supervised in their ability to Transition/Handover patient care until such a time that they have
demonstrated competency in the performance of this task. Programs must develop and utilize a method of
monitoring the Transition of Care/Handover process and update as necessary.
Revised 3/21
Reviewed 3/15, 5/17, 4/19, 2/23

95
Residents/Fellows Policies and Procedures Manual
SUPERVISION, PROGRESSIVE AUTHORITY AND RESPONSIBILITY OF
RESIDENTS/FELLOWS
Purpose: To set institutional standards for supervision of residents that ensures their education and our
compliance with ACGME institutional standards at the University of Connecticut School of Medicine and its
affiliated hospitals.
[Note: These standards are not meant to comply with standards required for billing purposes. Please see the
Medicare Guidelines for Teaching Physicians, Interns, and Residents]
Supervision in the setting of graduate medical education provides safe and effective care to patients;
ensures each resident/fellow’s development of the skills, knowledge, and attitudes required to enter the
unsupervised practice of medicine; and establishes a foundation for continued professional growth.
Ensuring adequate supervision of residents/fellows is the responsibility of the program director, faculty
physicians, departments, and the institution.
The following are standards for University of Connecticut School of Medicine resident/fellow positions,
irrespective of the affiliated site where the resident/fellow is training/working. These are minimum rules.
No program can fall below these standards, but they will be expanded if:
• Medical Staff rules at a given institution exceed these.
• Additional standards are required by The Joint Commission, CMS or any other regulatory body.
• An individual program has more stringent RC requirements for supervision.
• The clinical setting where the resident/fellow physician is training/working has additional rules.
Standards: Each patient must have an identifiable, appropriately credentialed and privileged attending
physician or licensed independent practitioner who is responsible and accountable for the patient’s care.
This information must be available to residents/fellows, faculty members, and other members of the health
care team.
All patient care performed by residents/fellows during training will be under the supervision of a physician
faculty member, a licensed provider, fellow, or a more senior resident, either on site, or by means of
telephonic and/or electronic modalities. Some activities require the physical presence of the supervising
faculty member. The specifics of this supervision must be documented in the medical record by the
supervising faculty member, licensed provider or supervising resident/fellow.
Residents/fellows, faculty members and licensed providers should inform their patients of their respective
roles in each patient’s care when providing direct patient care.
Levels of Supervision: Appropriate supervision of residents/fellows must be available at all times. The
program must demonstrate that the appropriate level of supervision in place for all residents is based on
each resident’s/fellow’s level of training and ability, as well as patient complexity and acuity. Supervision
may be exercised through a variety of methods, as appropriate to the situation.

96
Residents/Fellows Policies and Procedures Manual
• Direct Supervision: The supervising physician* is physically present with the resident during the
key portions of the patient interaction or the supervising physician and/or patient is not physically
present with the resident and the supervising physician is concurrently monitoring the patient care
through appropriate telecommunication technology.
• Indirect Supervision: The supervising physician is not providing physical or concurrent visual or
audio supervision but is immediately available to the resident for guidance and is available to
provide appropriate direct supervision.
• Oversight: The supervising physician is available to provide review of procedures/encounters with
feedback provided after care is delivered.
(*Supervising Physician: The supervising physician can be a faculty member or a more senior resident/fellow
than the resident needing supervision.)
Each resident/fellow must know the level of supervision required for them in all circumstances. PGY-1
residents must have, at all times, either direct or indirect supervision. Senior residents/fellows may serve
as a direct or indirect supervising physician for a more junior resident or fellow, based on the needs of the
patient and the skills of the individual resident or fellow as designated by the program director.
The supervising physician/licensed provider must be immediately available in person or by telephone 24
hours a day. Programs must ensure this occurs. Residents/fellows must know who the supervising
physician/licensed provider is and how to reach this individual. Schedules and contact information for
supervising physicians (faculty or more senior residents/fellows) and licensed providers must be readily
available to all parties involved with patient care.
Certain situations require communication between the resident/fellow and supervising attending. At a
minimum, the resident/fellow must notify the supervising attending physician /licensed provider of any
significant changes in the patient’s condition, including but not limited to:
• Patient admission to the hospital
• Transfer of a patient to a higher level of care including the intensive care unit
• Need for intubation or ventilator support
• Cardiac arrest or significant changes in hemodynamic status
• Development of significant neurological changes
• Development of major wound complications
• Medication errors requiring clinical intervention
• Any clinical problem that requires an invasive procedure or surgery
• Any condition which requires the response of a consulting team
• Change in code status
• Death
Supervision by Service:
Inpatient supervision: Every patient admitted to the hospital has an attending physician who is a member
of the hospital attending or affiliated medical staff. The attending physician will remain responsible for the
medical care of the patient in every aspect throughout the hospital stay of the patient unless the

97
Residents/Fellows Policies and Procedures Manual
responsibility is formally transferred to another service and this transfer is appropriately noted in the
patient’s medical record. When the attending physician is acting in the capacity of a supervisor, they must
obtain a comprehensive presentation for each admission from the resident/fellow. This includes a history
and physical exam. On the non-emergency admissions, charts shall contain a provisional diagnosis and plan
by the attending physician written no more than 7 days prior to the admission, or within twenty-four (24)
hours after admission. On all emergency patients, histories and physicals shall be recorded within 12 hours
after admission. In either case, the history and physicals must be written prior to any surgery. If the history
and physical is written by a resident/fellow, the attending physician shall review and authenticate the
resident’s/fellow’s history and physical examination within twenty-four (24) hours. The authentication
shall consist of the provider’s outline of the salient points of the history, physical, and management plan.
The attending physician must also require the resident/fellow to present the progress of each inpatient
daily, including discharge planning. While residents may write progress notes in patient’s charts, the
attending physician will also write appropriate progress notes documenting the portions of care they
specifically provide or supervise. Simply counter-signing a resident’s/fellow’s note is insufficient. All
required supervision must be documented in the medical record by the resident/fellow and the
supervising faculty member. The interval between practitioner’s progress notes shall not exceed three days
for non-critical nor daily for critical patients. Residents/fellows must communicate with the attending
physician to ensure that the orders they write are consistent with the attending physician’s medical
treatment plan for the patient. No countersignature by the attending physician is required for orders
written by a resident/fellow.
Outpatient supervision: The supervising physician/licensed provider must require residents/fellows to
present each outpatient’s history, physical exam and proposed diagnostic or treatment plan. All required
supervision must be documented in the medical record by the resident/fellow and the supervising
provider. (Exception to this is relevant for services which practice under Medicare’s Primary Care Exception
Rule). For services which have been approved to practice under Medicare guidelines, residents/fellows can
be supervised with Direct Supervision, Indirect Supervision, or Oversight depending on the
resident/fellow level and the supervision policy of the resident’s/fellow’s program.
Supervision of consultations: The supervising consulting attending/licensed provider must
communicate with the resident/fellow and obtain a presentation of the history, physical exam, and
proposed decisions for each consultation. This must be done within an appropriate time but no longer than
twenty-four (24) hours after notification of the consultation request. All required supervision must be
documented in the medical record by the resident and/fellow the supervising attending/licensed provider.
Supervision of procedures: The supervising attending must be certain that procedures performed by the
resident/fellow are warranted, that adequate informed consent has been obtained, and that the
resident/fellow has appropriate supervision during the procedure to include sedation.
• For procedures performed in the operating room, residents/fellows will always be supervised by
an attending physician for the key portions of the procedure.
• For procedures performed outside of the operating room, residents/fellows will be supervised by
an appropriately credentialed supervising physician or LIP. Again, the supervising physician can be
a faculty member or a more senior resident/fellow than the resident/fellow needing supervision

98
Residents/Fellows Policies and Procedures Manual
All required supervision must be documented in the medical record by the resident/fellow and the
supervising physician or LIP.
Supervision of emergencies: During emergencies, the resident/fellow should first and foremost provide
care for the patient and notify the supervising physician/licensed provider as soon as possible to present
the history, physical exam, and necessary diagnostic or treatment. All supervision must be documented in
the medical record by the resident/fellow and/or the supervising provider.
Progressive authority and responsibility for residents: Increasing responsibility for patient care is an
integral part of the medical education process. Specific roles and tasks for patient care must be assigned
by program directors and faculty members.
• Roles and responsibilities for residents/fellows are determined by the program director.
• Decisions regarding the level of supervision necessary for patient care provided by an individual
resident/fellow must be based on evaluation of that resident/fellow using specific criteria guided
by the Milestones.
• A faculty member acting in the capacity of a supervising attending physician must delegate portions
of patient care to residents/fellows based on the needs of the patient and the skills and experience
of the resident.
• Each resident/fellow must know the limits of his/her scope of authority and responsibility and the
circumstances under which varying levels of supervision apply.
Revised 6/17, 3/21, 12/21
Reviewed 4/19, 2/23
99
Residents/Fellows Policies and Procedures Manual
MOONLIGHTINGEXTRA CREDIT
Professional activities outside the program or “moonlighting” may be engaged in by residents/fellows only
with the permission of the Program Director. Program Directors must monitor the moonlighting activities
of their residents/fellows and residents/fellows must report their schedules for moonlighting. Written
permission must be placed in the resident’s/fellow’s file prior to engaging in any moonlighting activity.
Residents/fellows who engage in moonlighting activities without the knowledge and approval of the
Program Director may be considered for disciplinary action.
The following rules apply to moonlighting:
Residents/fellows cannot schedule any of these activities in such a way that they interfere with the
requirements of their program, duty hours, health or performance.
Moonlighting activities are not part of the malpractice liability coverage provided by the
residency/fellowship programs. Residents/fellows must obtain the appropriate license, liability
coverage, and DEA number for use in activities not related to the residency/fellowship.
Residents/fellows cannot moonlight in the capacity of an independent licensed practitioner in
activities related to his/her current training program.
All moonlighting activity counts towards resident/fellow duty hours (see Clinical and Educational
Work Hours Rules/Procedures).
Residents/fellows may not hold admitting privileges in any hospital or charge or receive fees for
professional services rendered as part of the residency/fellowship program.
Residents/fellows in J1 status are not allowed to moonlight.
In addition to moonlighting, some programs have extra credit activities within the program at any of the
University of Connecticut School of Medicine (UConn SOM) affiliated hospitals. These are activities that are
part of the educational program.
Hours spent on extra credit must be considered as part of the resident/fellow duty hours (see Clinical
and Educational Work Hours Rules/Procedures).
Hours spent on extra credit must be logged as appropriate in MyEvaluations.com, Kronos, etc. Extra
credit is monitored directly by the specific residency/fellowship Program Director as well as by the
Associate Dean of Graduate Medical Education (GME)and Designated Institutional Official (DIO)
Residents may not engage in extra credit when on leave, on a letter of deficiency or when the
resident/fellow is scheduled for vacation.
Extra Credit is covered by the malpractice liability coverage at each site.
PGY 1 residents are prohibited from participating in extra credit activities.
Residents in an approved research year can participate in moonlighting or extra credit with the program
director’s approval.
The Program Director or GME designee may prohibit moonlighting or extra credit. Moonlighting and extra
credit is prohibited if a resident/fellow is on a leave of absence for any reason, in remedial status or has a
letter of deficiency. Also, residents/fellows who have reached the end of their training period but
have not met requirements for receiving a certificate (i.e., Capital Area Health Consortium exit
interview, Institution Curriculum etc.) are NOT allowed to moonlight under the auspice of the
program or participate in extra credit activities.

100
Residents/Fellows Policies and Procedures Manual
Revised 1/15, 3/17, 4/19
Reviewed 3/21, 2/23
101
Residents/Fellows Policies and Procedures Manual
RESIDENT/FELLOW MISTREATMENT
The University of Connecticut (UConn) School of Medicine (SOM) is committed to a learning environment
of respect, collegiality, and collaboration. Our faculty commit to making sure each component of the
educational program is of the highest quality, must serve as role models, will support all students and fairly
evaluate and provide timely feedback.
Behaviors that impede a safe and effect learning environment are not tolerated. Across the SOM, we have
adopted the Compact Between Faculty and Undergraduate and Graduate Medical Trainees.
The following process on Resident/Fellow Mistreatment is an affirmation of the importance of this issue
with expectations to respect race, gender, religion, sexual orientation, age, disability, and other protected
classes of individuals along with diversity of opinion, socioeconomic status and unique individuality within
our community. The learning environment will be free of belittlement, humiliation, hostility, or personal
judgment. This policy is meant to compliment the institutional policy against discrimination, harassment
and related interpersonal violence (see Prohibition of Discrimination and Discriminatory Harassment,
Including Sexual Harassment and Sexual Assault, Intimate Partner Violence, and Stalking).
Definition of Mistreatment
The AAMC defines mistreatment as follows:
“Mistreatment arises when behavior shows disrespect for the dignity of others and unreasonably
interferes with the learning process. It can take the form of physical punishment, sexual harassment,
psychological cruelty, and discrimination based on race, religion, ethnicity, sex, age or sexual orientation.”
Reporting Mistreatment
Residents/Fellows may report mistreatment via several avenues
See the Reporting Concerns Policy
Protection from Retaliation
Retaliation against any individual who, in good faith, reports or participates in the reporting, investigation,
or adjudication of mistreatment is strictly forbidden.
See the University’s Non-Retaliation Policy
Revised 4/19, 1/21
Reviewed 3/21

102
Residents/Fellows Policies and Procedures Manual
COUNSELING SERVICES
Medical residents/fellows at the University of Connecticut School of Medicine (UConn SOM) have available
to them consultation and/or counseling services.
A resident/fellow may choose to utilize the Employee Assistance Program (EAP) or the privately practicing
mental health providers listed below. The Capital Area Health Consortium (CAHC) provides these services
at no cost to the resident/fellow. There is no need for a resident/fellow to notify his/her Program Director,
the CAHC or their health insurance carrier when accessing the Employee Assistance Program (EAP) and
the Mental Health Services listed below.
A resident/fellow also may opt to utilize a provider of his/her choosing at their own expense and/or
through their health insurance carrier.
Residents/fellows also have access to urgent or emergent care 24 hours a day, seven days a week through
the emergency department at local hospitals. CAHC will not cover the emergency room copayment cost.
Employee Assistance Program (EAP)
All residents/fellows may contact the EAP at UConn Health to access counseling services from
psychologists, social workers, and other counselors. There is no limit to the number of sessions provided.
UConn Health Employee Assistance Program, 860-679-2877
http://health.uconn.edu/occupational-environmental/employee-assistance-program/
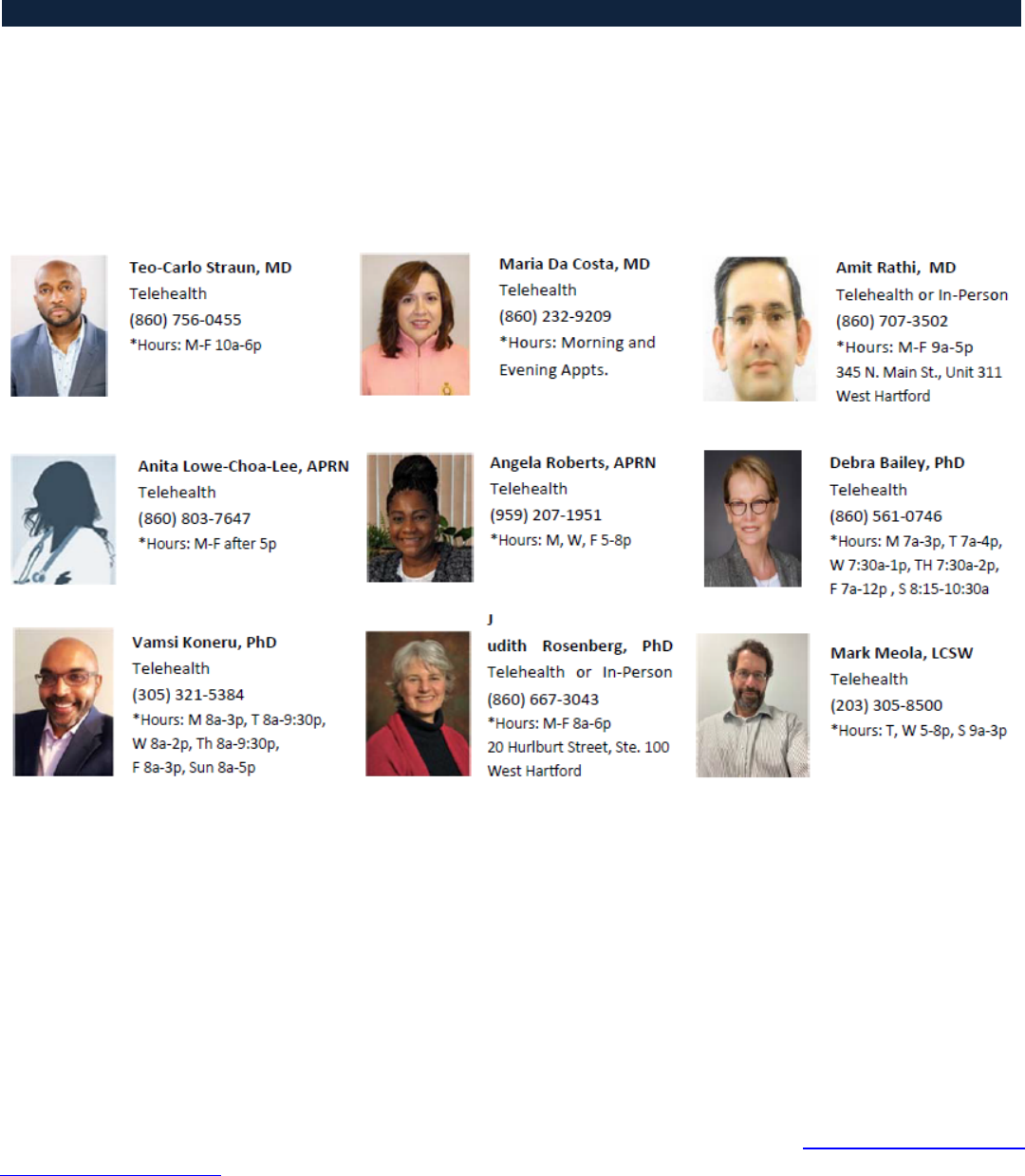
103
Residents/Fellows Policies and Procedures Manual
Mental Health Services
Mental health providers are available to counsel Capital Area Health Consortium (CAHC) employed medical
residents/fellows. Residents/fellows may contact one of these providers as desired. Residents/fellows
must identify themselves as resident/fellow employees of the CAHC at the time of initial contact. To verify
employment, the resident/fellow must bring a pay stub to the first appointment.
Unless a resident/fellow participating in these services has been referred by the UConn School of Medicine
due to some performance-related concern, these services will be provided in a confidential manner.
Health Assistance Intervention Education Network (HAVEN)
A resident/fellow may also choose to access the Health Assistance Intervention Education Network
(HAVEN).
HAVEN is the health and wellness program authorized by state law to serve healthcare professionals in
Connecticut. HAVEN provides a safe environment for coordinating educational, rehabilitative, and
supportive services for concerns related to alcoholism, substance abuse, behavioral or mental health issues
and/or physical illness. Residents/fellows may self-refer to HAVEN for evaluation and treatment. In some
instances, residents/fellows may undergo a mandated evaluation by HAVEN (see Fit for Duty/Employee
Assistance Evaluations). The Office of Graduate Medical Education must be notified when a resident/fellow
self-refers or is referred to HAVEN. This notification can be made by the resident/fellow or by HAVEN once
authorized by the resident/fellow to do so.
104
Residents/Fellows Policies and Procedures Manual
While the resident/fellow is participating in a UConn SOM residency/fellowship program and employed
by the CAHC, the initial evaluation by HAVEN and related costs will be paid in full by CAHC. If an ongoing
treatment plan is needed, the resident/fellow will be expected to pay 10% of the monthly fee of HAVEN.
The resident/fellow is eligible for reimbursement of the biologic testing fees once they have paid $500 per
year out of pocket. The resident/fellow will be reimbursed by the CAHC for expenses incurred above this
amount upon submission of all receipts/documentation of payment to the CAHC. Receipts must be
submitted within 60 days to be eligible for reimbursement. Residents/fellows will not be reimbursed for
provider copays, mobile laboratory fees, emergency department laboratory fees, shipping costs for test
kits. If a resident/fellow self-refers or is undergoing a mandatory evaluation to HAVEN, they must contact
the CAHC in order for the CAHC to process payments to HAVEN.
HAVEN staff will make recommendations about further treatment and when appropriate will work with
the UConn School of Medicine (UConn SOM) Graduate Medical Education (GME) Office designee and the
Program Director in identifying whether or not the resident/fellow is fit for duty.
Contact information is:
HAVEN
1210 Mill Street
East Berlin, CT 06023
Telephone: (860) 828-3175
Confidential Fax: (860) 828-3192
http://haven-ct.org/
Other Counseling Services
AnthemLive Health Psychology Program provides convenient access to licensed Psychologists and
Therapists available 7 days a week in the privacy of your own home. Their trained professionals can
assist with a variety of conditions, including stress, anxiety, depression, grief and relationship or family
issues. There is no copay for these services.
Anthem LiveHealth Psychology
Guardian WorkLifeMatters Employee Assistance Program provides up to 3 free counseling sessions for
support services to help promote well-being and enhance the quality of life for you and your family. A
free consultation with an attorney and discounts on legal services thereafter as well as financial planning
tools and assistance is also available.
Guardian Employee Assistance Program
Revised 9/17, 3/20, 11/20, 12/21, 3/22, 4/22, 8/22, 10/22, 1/23, 4/23, 7/23, 10/23, 6/24
Reviewed 3/21

105
Residents/Fellows Policies and Procedures Manual
UCONN OMBUDS OFFICE
The UConn Ombuds Officer serves as a neutral resource who provides confidential and informal assistance
to members of the UConn Health community. The Ombuds Office was established to provide a confidential,
neutral resource for staff, faculty, professional and graduate students, and residents/fellows to express
concerns, identify options to address workplace conflicts, facilitate productive communication, and surface
responsible concerns regarding university policies and practices.
Residents/fellows may contact the Ombuds Officer when a confidential conversation or source of
information may be needed. The role of the Ombuds is to listen to concerns, provide information about
University policies, help evaluate situations, and assist in making plans to address issues or conflicts.
Contacting the Ombuds Office is completely voluntary.
The Ombuds Office at UConn Health is located in Room TG109 on the main entrance floor of the University
Tower. The office is adjacent to the Patient Registration and Information desk to the left of the hospital
entrance.
More information and contact information can be found in the link below:
https://ombuds.uconn.edu/
Created 4/19
Revised 3/21
Reviewed 2/23
106
Residents/Fellows Policies and Procedures Manual
FIT FOR DUTY/EMPLOYEE ASSISTANCE EVALUATIONS
When a resident/fellow has been identified as having academic deficiencies or as exhibiting behavior or
conduct or as having any condition or circumstance which the Program Director reasonably believes are
interfering or could interfere with the resident/fellow’s performance and/or prevent them from properly
performing their responsibilities in the program, the resident/fellow may be required to undergo a
mandated evaluation regarding Fitness for Duty. The type of the evaluation will be determined by the
Program Director in consultation with the Graduate Medical Education (GME) Office. The resident/fellow
may be required to have either a mandated evaluation with the Employee Assistance Program (EAP)
evaluation to determine the need for a formal Fit for Duty evaluation, or the resident/fellow may be
required at the outset to undergo a formal Fit for Duty either with an appropriate health care provider who
may be a psychiatrist, psychologist, the HAVEN* program, or other suitable provider. These evaluations
may be used to determine if a resident’s/fellow’s performance is being or may be affected by impairment
that includes but is not limited to medical conditions, mental health conditions, emotional disorders,
and/or substance abuse problems. The purpose of an evaluation is to determine the resident’s/fellow’s
ability to meet the academic expectations of his/her program and/or to perform his/her clinical duties and
responsibilities safely, without danger to patients, colleagues, or self.
Concerns regarding a resident’s/fellow’s Fit for Duty must be discussed with the Associate Dean for GME,
DIO, or Assistant DIO. The Assistant DIO should be the first contact to discuss a concern.
EAP Evaluation
If a mandated EAP evaluation is needed, the resident/fellow will be placed on Administrative Leave (see
Administrative Leave Policy) by the Program Director/designee and referred to the University of
Connecticut’s EAP office. The Associate Dean for GME, DIO or Assistant DIO, and/or the Program Director
will contact the Employee Assistance Program (EAP) director. As this is a mandated EAP evaluation, the
Program Director and/or the Associate Dean for GME, DIO, or Assistant DIO will share information
regarding the concerns with EAP personnel. This is not a confidential session between the resident/fellow
and EAP personnel. Therefore, the evaluation with any recommendations resulting from the evaluation
will not be subject to the same privacy rules as occur in a therapeutic relationship. The Program Director
and the Associate Dean for GME, DIO, or Assistant DIO will be notified by EAP personnel regarding the
outcome of the evaluation.
If it is determined on the basis of or in conjunction with the EAP evaluation that the resident/fellow
requires a formal Fit for Duty evaluation, EAP personnel will notify the Program Director and the
Associate Dean for GME, DIO, or Assistant DIO of their recommendation in writing. The
resident/fellow will be mandated to comply with this recommendation (see below re: Fit for Duty
evaluations).
If it is determined from the EAP evaluation that the resident/fellow is able to work and does not
need a formal Fit for Duty evaluation, EAP personnel will notify the Program Director and the
Associate Dean for GME, DIO, or Assistant DIO in writing. In some instances, EAP personnel may
recommend further evaluation/management/treatment by a health care provider (physician,
masters of social work, psychologist, psychiatrist, etc.). While the Program Director cannot mandate
compliance with said recommendation, it will be strongly encouraged.

107
Residents/Fellows Policies and Procedures Manual
Fit for Duty Evaluation
If it is determined by the Program Director in consultation with the Associate Dean for GME, DIO, or
Assistant DIO, and/or EAP that a formal Fit for Duty evaluation is necessary, or if a formal Fit for Duty
evaluation is recommended by EAP personnel, the resident/fellow will be placed on or remain on
Administrative Leave until their fitness for duty is determined (see Administrative Leave Policy). The
resident/fellow may then be referred to an appropriately qualified healthcare provider (e.g. a psychiatrist,
psychologist, the HAVEN program, or other suitable provider) for assessment depending on the nature of
the concern. As this is a mandated formal Fit for Duty evaluation, the Program Director and/or Associate
Dean for GME, DIO, or Assistant DIO will share information with the psychiatrist or the HAVEN personnel.
This is not a confidential session between the resident/fellow and a provider and therefore the evaluation
will not be subject to the same privacy rules as occur in a therapeutic relationship. The Program Director
and the Associate Dean for GME, DIO, or Assistant DIO will be notified of the outcome of the formal Fit for
Duty evaluation in writing.
The formal Fit for Duty evaluation may determine that the resident/fellow is fit to return to work
with or without accommodations and/or with or without additional treatment and/or participation
in a regimen or program. The resident/fellow will be promptly notified of the outcome of the fit for
duty evaluation. In order for a resident/fellow to return to the program, a written fit for duty report
must be submitted by the provider to the Program Director and the Associate Dean for GME, DIO,
or Assistant DIO. Upon receipt of the report and review of any requested accommodations/needs
of the resident/fellow, the Associate Dean for GME, DIO, or Assistant DIO shall consider whether to
return the resident/fellow to work, with or without some or all aspects of any recommended
treatment and/or accommodation and/or restrictions on participation in the program. As part of
this process, the resident/fellow will be afforded an opportunity to provide input to the Associate
Dean for GME, DIO, or Assistant DIO, and the Program Director.
If a resident/fellow is determined not to be fit for duty, the provider will contact the Program
Director and the Associate Dean for GME, DIO, or Assistant DIO in writing. The resident/fellow will
also be promptly notified of the outcome of the Fit for Duty evaluation. The Program Director in
consultation with the Associate Dean of GME, DIO, or Assistant DIO will then determine the status
of the resident/fellow in the program. As part of this process, the resident/fellow will be afforded
an opportunity to provide input to the Associate Dean for GME, DIO, or Assistant DIO, and the
Program Director regarding his/her status in the program.
The status of a resident/fellow who is not deemed fit to return to training after twelve (12) weeks will be
determined by the Program Director in consultation with the GME Office. The position of the
resident/fellow may or may not be held.
The resident/fellow will be promptly notified of the outcome of all evaluations and all decisions regarding
his or her leave and status in the program.
The Fit for Duty evaluation of a resident/fellow will be paid in full by the Capital Area Health Consortium
(CAHC).

108
Residents/Fellows Policies and Procedures Manual
A resident/fellow who refuses a Fit for Duty Evaluation or who does not comply with all required
appointments, evaluations, or other program conditions will not be allowed to work as a resident/fellow,
and such refusal/noncompliance may be cause for termination/dismissal.
*HAVEN is the health and wellness program authorized by state law to serve healthcare professionals in
Connecticut. HAVEN provides a safe environment for coordinating educational, rehabilitative, and
supportive services for concerns related to alcoholism, substance abuse, behavioral or mental health
issues, and/or physical illness.
Revised 4/16, 3/17, 4/19, 3/21, 1/23

109
Residents/Fellows Policies and Procedures Manual
SECTION IV: PERFORMANCE EVALUATIONS
110
Residents/Fellows Policies and Procedures Manual
MILESTONES
The Milestones represent a roadmap for the development of residents and fellows as they advance in clinical
skills, knowledge, and values. The Milestones are divided into the six Core Competencies of Patient Care,
Medical Knowledge, Professionalism, Interpersonal and Communication Skills, Practice-based Learning and
Improvement, and Systems-based Practice. Each Core Competency is divided into Subcompetencies laid out
in five levels.
Each specialty has been tasked with crafting its own Milestones. Indeed, the patient care skills for an internal
medicine resident will differ from those for an interventional radiology fellow. The specialty-specific Milestones
guide the learning and assessment of learners in that specialty or subspecialty.
From Level 1 to Level 5, the Milestones describe a stepwise progression towards achieving mastery using the
Dreyfus Model of Development as a foundation. Level 1= Novice (a starting resident or fellow); Level 2=
advanced beginner; Level 3= competent; Level 4= proficient; Level 5=expert. Level 4 is a graduation target, but
not an absolute requirement of the ACGME; each program or institution sets the requirements for graduation.
Level 5 describes aspirational performance for a resident or fellow who is acting as a role model or coach for
others.
Summary Recommendations for Residents and Fellows
1.
Be sure to review the specialty Milestones on an ongoing basis, especially at the start of each
academic year, to help in professional development.
2.
Perform a self-assessment twice a year around the same time the program’s Clinical Competency
Committee (CCC) meets.
3.
Review and compare the self-assessment with the CCC’s Milestone ratings with your program
director, faculty advisor, or mentor.
4.
Write an individualized learning plan at least twice a year, and discuss it with the program director,
faculty advisor, or mentor.
5.
Be an active participant in regular assessment and feedback.
Milestones Can Help with Assessing Oneself and Growing as a Physician
Residents and fellows should use the Milestones as they consider where they are in their educational program, to
identify areas to grow, and to understand what each stage looks like. Often the Milestones describe a progression
from common or basic abilities to more complex and nuanced ones.
Created 2/23
111
Residents/Fellows Policies and Procedures Manual
EVALUATION AND PROMOTION
Evaluation
The University of Connecticut School of Medicine (UConn SOM) recognizes learning on a continuum
from a beginner to a competent physician. The primary responsibility for defining the standards of
academic performance and personal and professional development rests with individual programs and
their Program Director.
Each UConn SOM residency/fellowship program will provide formative and summative evaluations of
residents’/fellows’ performance in the Milestones and in each of the six ACGME Core Competencies for
their level of training. Written evaluations are provided to residents/fellows according to the program’s
evaluation process. At the conclusion of training, the Final Verification of Training Form, a summative
evaluation, is provided to the resident/fellow. The Final Verification of Training Form must be signed
by both the Program Director and the resident/fellow. The original is provided to the Graduate Medical
Education (GME) Office.
Each program must have a Clinical Competence Committee (CCC). The CCC reviews resident/fellow
evaluations at least quarterly and the Program Director/designee will meet and evaluate all
residents/fellows biannually. The CCC serves in an advisory role to the Program Director to determine
the status of each resident/fellow in all aspects of their training program.
Promotion
Each program must have a policy that determines the criteria for promotion of a resident/fellow. The
Program Director determines if a resident/fellow has successfully met those requirements. If a
resident/fellow is making sufficient progress towards promotion, the Program Director will submit the
resident’s/fellow’s name to the GME Office to indicate that a contract may be issued to the
resident/fellow for the subsequent year of training. This contract is conditional upon the
resident/fellow meeting the milestones and criteria for promotion as determined by the Program
Director. In the final year of training, the Program Director will submit the resident’s/fellow’s name to
the GME Office to indicate that a resident/fellow will graduate from the program. Graduation from the
program requires the resident/fellow to meet all of the criteria for graduation as determined by the
Program Director.
If a Program Director determines that a resident/fellow is not meeting criteria for promotion, the
Program Director has several options. See the policies on Academic Deficiencies Review Procedures
and Code of Conduct Violations/Non-Academic Deficiencies Review Procedures for further details.
Revised 4/17, 4/19, 3/21
Reviewed 2/23
112
Residents/Fellows Policies and Procedures Manual
ACADEMIC DEFICIENCIES REVIEW PROCEDURES
Status Options for a Resident/Fellow with an Academic Deficiency
It is expected that all residents/fellows progress according to criteria set by the program. The Program
Director will determine, on a case-by-case basis, which of the following is most appropriate to address
perceived deficiencies in academic performance for a particular resident/fellow. The options for an
academic deficiency are a Letter of Remediation (LoR), a Letter of Deficiency (LoD), and a Letter of
Deficiency with Adverse Action (LoDAA).
Adverse Actions include:
Delayed promotion of a resident/fellow with extension of contract/appointment
Non-renewal of contract/appointment
Termination/dismissal
Of note:
A resident/fellow who is being formally remediated with either a Letter of Remediation or a Letter
of Deficiency without Adverse Action at the time of promotion or at the time of completion of the
program is by definition not meeting the standards of the program and therefore cannot be
promoted to the next level of training or complete the program. Therefore, this must result in an
Adverse Action (see Letter of Deficiency with Adverse Action). All Adverse Actions will be reflected
on the Final Residency/Fellowship Training Summary Verification form.
If an Adverse Action is delayed promotion or non-renewal, a resident/fellow may remain in the
training program during the appeal process at the discretion of the Program Director in
consultation with the GME Office. If a resident/fellow remains in the training program during the
appeal process, they will receive pay and benefits. If the resident/fellow does not remain in the
training program during the appeal process, they will not receive pay but benefits will continue
through the appeals process.
If a resident/fellow is terminated/dismissed, they will not receive pay, but benefits will continue
throughout the appeal process.
If an Adverse Action of termination/dismissal is rescinded at any level of appeal, the
resident/fellow will rejoin the training program. Pay will be reinstated and will be retroactive to
the termination/dismissal date.
If an Adverse Action of delayed promotion, non-renewal or termination/dismissal is rescinded at
any level of appeal, the resident/fellow will return in any remedial status in existence prior to the
Adverse Action.
The options for a Program Director when a resident/fellow is identified as having an academic deficiency
are described below.
Letter of Remediation
The Office of Graduate Medical Education must be contacted by the Program Director as soon as it is
determined that a Letter of Remediation may be required.
A resident/fellow whose academic performance does not meet program standards in one or more of the
competencies defined by the Accreditation Council for Graduate Medical Education (ACGME) may be given
113
Residents/Fellows Policies and Procedures Manual
a Letter of Remediation to meet the program’s standards. This status is not appealable. A period of
remediation outlined in an LoR should not last longer than one month absent extenuating circumstances
in consultation with the Office of Graduate Medical Education. A resident/fellow cannot be promoted to
the next level of training while on a Letter of Remediation.
Before the decision is made to place a resident/fellow on a Letter of Remediation, the Program Director
will meet with the resident/fellow to discuss observed deficiencies. At this juncture, the resident/fellow
must be offered the opportunity to provide input and/or information to the Program Director regarding
the observed deficiencies. To the extent the Program Director’s decision to place a resident/fellow on a
Letter of Remediation is a decision that is made with input from the Clinical Competency Committee or any
other committee, any mitigating information provided by the resident/fellow must be shared with the
Clinical Competency or other committee prior to the decision.
The Letter of Remediation must be delivered to the resident/fellow within 3 business days of the decision
to issue the Letter of Remediation and in a manner which requires a signed and dated receipt of delivery
to the resident/fellow and a witness signature.
If the remediation is successful and there are no further concerns in training this status will not be reflected
on the Final Residency/Fellowship Training Summary Verification form.
The resident’s/fellow’s program file will include the following:
Documentation of (1) the meeting (s) to discuss the deficiencies, remediation plan and expectations,
and (2) delivery of a Letter of Remediation to the resident/fellow
Documentation of outcome after Remediation:
o Successful remediation of the deficiencies or
o Transition to a Letter of Deficiency (LoD) or a Letter of Deficiency with Adverse Action
(LoDAA)
Letter of Deficiency (LoD)
The Office of Graduate Medical Education must be contacted by the Program Director as soon as it is
determined that a Letter of Deficiency may be required.
A Letter of Deficiency (LoD) is a formal written notification of deficiency in one or more of the ACGME
competencies. A Program Director may choose to address deficiencies with a of Remediation first, but is
not required to use a Letter of Remediation first if the Program Director determines that an LoD may be
warranted. This status is not appealable. A resident/fellow may not be promoted to the next level of
training while on an LoD.
Before the decision is made to give a resident/fellow an LoD, the Program Director must meet with the
resident/fellow and address the observed deficiencies. At this juncture, the resident/fellow must be
offered the opportunity to provide input and/or information to the Program Director regarding the
observed deficiencies. To the extent the Program Director’s decision to issue a resident/fellow a Letter of
Deficiency is a decision that is made with input from the Clinical Competency Committee or any other
committee, any mitigating information provided by the resident/fellow must be shared with the Clinical
Competency or other committee prior to the decision.
114
Residents/Fellows Policies and Procedures Manual
The LoD must be delivered to the resident/fellow within 3 business days of the decision to issue the LoD
and in a manner which requires a signed and dated receipt of delivery to the resident/fellow and a witness
signature.
If the remediation is successful and there are no further concerns in training, this status will not be
reflected on the Final Residency/Fellowship Training Summary Verification form.
The resident’s/fellow’s program file will include the following:
Documentation of (1) the meeting(s) to discuss the deficiencies, remediation plan and expectations,
and (2) delivery of the LoD to the resident/fellow
Documentation of outcome:
o Successful remediation of the deficiencies or
o Transition to a Letter of Deficiency with Adverse Action (LoDAA)
Letter of Deficiency with Adverse Action (LoDAA)
The Office of Graduate Medical Education must be contacted by the Program Director as soon as it is
determined that a Letter of Deficiency with Adverse Action may be required.
A Letter of Deficiency with Adverse Action is a formal written notification of deficiency in one or more of
the ACGME competencies. A Program Director may determine that an LoDAA is necessary after a Letter of
Remediation; after an LoD; or an LoDAA may be the first step in addressing deficiencies. An LoDAA is
required if a resident/fellow does not make adequate progress as outlined during a period of time with an
LoD.
Adverse Actions include:
Delayed promotion of a resident/fellow with extension of contract/appointment
Non-renewal of contract/appointment
Termination/dismissal
Adverse Actions, not the Letter of Deficiency, are appealable. A resident/fellow who receives an LoDAA
must be provided with access to the appeals process.
Before the decision is made to give a resident/fellow an LoD with Adverse Action, the Program Director
must meet with the resident/fellow and address the observed deficiencies. The resident/fellow must be
informed of any Adverse Action that is being considered. At this juncture, the resident/fellow must be
offered the opportunity to provide input and/or information to the Program Director regarding the
observed deficiencies. To the extent the Program Director’s decision to issue a resident/fellow an LoDAA
is a decision that is made with input from the Clinical Competency Committee or any other committee, any
mitigating information provided by the resident/fellow must be shared with the Clinical Competency or
other committee prior to the decision.
The LoDAA must be delivered to the resident/fellow within 3 business days of the decision to issue the
LoDAA and in a manner which requires a signed and dated receipt of delivery to the resident/fellow and a
witness signature.
The resident’s/fellow’s program file will include the following:
115
Residents/Fellows Policies and Procedures Manual
Documentation of (1) the meeting(s) to discuss the observed deficiencies and the Adverse Action
(2) delivery of the LoDAA to the resident/fellow, and (3) documentation that the resident/fellow
was provided with information regarding how to access to the appeals process
Documentation of outcome:
o Successful remediation of the deficiencies when the Adverse Action is extension of training
or
o Non-renewal of contract/appointment or
o Termination/dismissal
The status of a resident/fellow with an LoDAA will be reflected on the Final Residency/Fellowship Training
Summary Verification form.
A Letter of Deficiency with an Adverse Action may not be removed from a resident’s/fellow’s official GME
file.
Appeal of Academic Adverse Actions
A resident/fellow is entitled to appeal an Adverse Action. At each level of appeal, the charge of the person
or committee hearing the appeal is to determine if (1) appropriate process was followed and (2) the
decision to impose an Adverse Action was made on reasonable grounds. At each level of appeal, the person
or committee hearing the appeal will either rescind or uphold the Adverse Action.
If an Adverse Action is upheld at any level of appeal, the resident/fellow must be informed about his/her
right to appeal this decision to the next level of appeal.
If an Adverse Action of extension of training is rescinded at any level of appeal, the Adverse Action will be
removed from the Letter of Deficiency. The resident/fellow must still adhere to the required remediation
plan and successfully remediate the deficiencies outlined in the LoD. In this situation, because the Adverse
Action is removed from the LoD, this status will not be reflected on the Final Residency/Fellowship
Training Summary Verification form.
If an Adverse Action of non-renewal of contract or termination is rescinded at any level of appeal, the
Adverse Action will be removed from the Letter of Deficiency. The Program Director, at his or her
discretion, may amend the Letter of Deficiency to include a required remediation plan or to add additional
requirements to the Letter of Deficiency. In this situation, because the Adverse Action is removed from the
LoD, this status will not be reflected on the Final Residency/Fellowship Training Summary Verification
form.
If the Adverse Action is upheld upon appeal, the status of a resident/fellow with an LoDAA will be reflected
on the Final Residency/Fellowship Training Summary Verification form.
The timelines outlined in the appeals process that follows may be adjusted if agreed upon by all parties.

116
Residents/Fellows Policies and Procedures Manual
Level 1: Appeal to the Department Chair, Department Designee* or GME Designee**
The resident/fellow has the right to appeal the Adverse Action. The first level of appeal is to the Department
Chair. If the Department Chair sits on the CCC, or if the Department Chair is the Program Director, or if the
Department Chair must recuse themselves due to any conflict, the resident/fellow appeal is to a
Department Designee. If an appropriate Department designee is not identified, the resident/fellow appeal
is to a GME Designee.
The resident/fellow must notify the Department Chair or Department or GME Designee of his/her request
to appeal in writing within three (3) business days of receiving the LoDAA. The Department Chair or
Department or GME Designee must acknowledge receipt of the appeal in writing to the resident/fellow.
Email is acceptable.
The resident/fellow and the Program Director must submit any documents they wish to be considered for
the appeal to the Office of Graduate Medical Education within five (5) business days of the appeal request.
The Department Chair or the Department or GME Designee must meet with the resident/fellow and any
additional sources (i.e., the Program Director, other faculty, staff, etc.) as they deem appropriate within ten
(10) business days of receiving the documents. The resident/fellow will be given an opportunity to provide
input at his/her meeting with the Department Chair or Department or GME Designee prior to any decision
being made.
The Department Chair or the Department or GME Designee must reach a decision regarding the appeal and
must deliver said decision in writing to the resident/fellow and the Program Director within three
(3) business days of concluding the review. The decision must be delivered in a manner which requires
a signed and dated receipt of delivery to the resident/fellow.
The resident/fellow must sign and date the written decision to acknowledge receipt of said document
within two (2) business days and deliver the signed copy to the Department Chair or Department or GME
Designee and to the Office of Graduate Medical Education. If the resident/fellow fails to do so, it will be so
noted in resident’s/fellow’s program file.
Level 2: Appeal to the Associate Dean for Graduate Medical Education/Designee**
The resident/fellow has the right to appeal the decision of the Department Chair or Department or GME
designee. The second and final level of appeal is to the Associate Dean for Graduate Medical Education. If
the Associate Dean for Graduate Medical Education must recuse themselves from the appeal, the appeal
will be to a GME Designee. The Associate Dean for Graduate Medical Education or GME Designee will
convene an ad hoc committee to hear the appeal. The ad hoc committee is advisory to the Associate Dean
for Graduate Medical Education or GME Designee.
The resident/fellow must notify the Associate Dean for Graduate Medical Education or the GME Designee
of his/her request to appeal in writing within three (3) business days of receiving the written decision of
the Department Chair or Department or GME Designee. The Associate Dean for Graduate Medical Education
or GME Designee must acknowledge receipt of the appeal in writing to the resident/fellow. Email is
acceptable.

117
Residents/Fellows Policies and Procedures Manual
The resident/fellow and the Department Chair or Department or GME Designee from Level 1 of the appeal
must submit documents they wish to be considered for the appeal to the Office of Graduate Medical
Education within five (5) business days of the appeal request.
The Associate Dean for Graduate Medical Education or GME Designee and the members of the ad hoc
committee must meet with the resident/fellow and any additional sources (i.e., the Program Director, other
faculty, staff, etc.) as they deem appropriate within ten (10) business days of receiving the documents. The
resident/fellow will be given the opportunity to provide input at his/her meeting with the ad hoc
committee and Associate Dean for Graduate Medical Education or GME Designee prior to any decision
and/or recommendation being made.
The Associate Dean for Graduate Medical Education or GME Designee must reach a decision regarding the
appeal and must deliver said decision in writing to the resident/fellow and the Program Director
within three (3) business days of concluding the review. The decision must be delivered in a manner which
requires a signed and dated receipt of delivery to the resident/fellow.
The resident/fellow must sign and date the written decision to acknowledge receipt of said document
within 2 business days and deliver the signed copy to the Associate Dean for Graduate Medical Education
or GME Designee and to the Office of Graduate Medical Education. If the resident/fellow fails to do so, it
will be so noted in the resident’s/fellow’s program file.
*The Department Designee will be a faculty member of the resident’s/fellow’s Department. This
faculty member may not be a member of the Clinical Competency Committee of the residency or
fellowship program, nor may they be the advisor assigned to the resident/fellow. This faculty
member cannot have had any prior involvement with the resident’s/fellow’s situation that led to
the contemplated Letter of Deficiency with Adverse Action unless this requirement is not possible.
The Department Designee will be selected by the Designated Institutional Official (DIO).
** The GME designee will be a voting member of the GMEC. This individual cannot be faculty in the
resident’s/fellow’s training program, nor can they have any prior involvement with the
resident’s/fellow’s situation that led to the contemplated Letter of Deficiency with Adverse Action
unless this requirement is not possible The GME designee will be selected by the Designate
Institutional Official (DIO).
The Dean of the School of Medicine will be notified of the final decisions of the Associate Dean for
Graduate Medical Education or GME Designee regarding adverse actions. The Dean of the School of
Medicine will also be notified if there is no appeal of an Adverse Action.
Revised 10/22, 7/24
118
Residents/Fellows Policies and Procedures Manual
CODE OF CONDUCT VIOLATIONS/NON-ACADEMIC DEFICIENCIES REVIEW
PROCEDURES
The University of Connecticut School of Medicine (UConn SOM) and all of its major affiliates have codes of
conduct that apply to resident/fellow participation in program related duties wherein residents/fellows
are expected to act in a professional, courteous, respectful, and confidential manner. The resident/fellow
contract states that residents/fellows shall abide by all rules, regulations and bylaws of the program,
clinical department, and institution in which they are assigned. Violating these rules may be cause for
disciplinary action up to and including dismissal.
All Code of Conduct Violations have the potential to interfere with a resident’s/fellow’s performance and
therefore may interfere with a resident’s/fellow’s ability to meet the expectations and requirements of a
resident’s/fellow’s academic program and employment.
Program Directors, faculty, other residents/fellows, patients and any other individual who has contact with
resident/fellow physicians can report suspected Code of Conduct violations. If there is an allegation of a
Code of Conduct violation, the Program Director, the DIO/designee and the Associate Dean of Graduate
Medical Education (GME) will be notified. An allegation of a Code of Conduct violation will be investigated
by the Program Director. If the alleged Code of Conduct violation is sufficiently serious, the DIO/designee
may, at his/her discretion, conduct the investigation in lieu of the Program Director. When appropriate,
the Office of Institutional Equity and/or law enforcement may also be involved in the investigation of an
alleged Code of Conduct violation. When the Office of Institutional Equity and/or law enforcement
investigate an alleged Code of Conduct violation that falls within their purview, they will provide a report
of their findings to the individual conducting the investigation.
During the period of investigation, it may be necessary to remove a resident/fellow from active
participation in the clinical and educational responsibilities of the program (see Administrative Leave
Policy).
In the course of an investigation of an alleged Code of Conduct violation, those investigating the alleged
Code of Conduct violation (the Program Director or the DIO/designee) will meet with the resident/fellow
after providing notice in order to provide the resident/fellow the opportunity to be heard regarding the
alleged violation. To the extent that the Clinical Competency Committee (CCC) or any other committee
will provide input into the decision of whether or not to substantiate the Code of Conduct violation, any
mitigating or other information provided by the resident/fellow must be shared with the Clinical
Competency or other committee. Prior to the meetings, the resident/fellow will be given written notice of
the alleged Code of Conduct violation and the potential consequences of a substantiated violation. These
meeting (s) and/or attempt(s) to meet will be documented.
If a resident/fellow has been placed on Administrative Leave due to a reported or suspected Code of
Conduct violation, and the alleged Code of Conduct violation is not substantiated, the resident/fellow will
return to the program unless any other leave status applies.
When the alleged Code of Conduct violation is investigated by the Program Director, the Program Director,
in consultation with the DIO/designee, will determine if the Code of Conduct violation is substantiated by

119
Residents/Fellows Policies and Procedures Manual
a preponderance of the evidence. The Program Director will meet with the resident/fellow to inform them
of the outcome of the investigation. The Program Director, in consultation with the DIO/designee, will
decide if the resident/fellow is to receive a Letter of Misconduct (LoM). If so, the options are a Letter of
Misconduct (LoM) or a Letter of Misconduct with Adverse Action (LoMAA).
When the alleged Code of Conduct violation is investigated by the DIO/designee, they will determine if
the Code of Conduct violation is substantiated by a preponderance of the evidence. The DIO/designee will
meet with the resident/fellow to inform them of the outcome of the investigation. The DIO/designee, in
consultation with the Program Director, will decide if the resident/fellow is to receive a Letter of
Misconduct (LoM). If so, the options are a Letter of Misconduct (LoM) or a Letter of Misconduct with
Adverse Action (LoMAA).
Adverse Actions include:
Delayed promotion of a resident/fellow with extension of contract/appointment
Non-renewal of contract/appointment
Termination/dismissal
Of note:
All Adverse Actions will be reflected on the Final Residency/Fellowship Training Summary
Verification form.
If an Adverse Action is delayed promotion or non-renewal, a resident/fellow may remain in the
training program during the appeal process at the discretion of the Program Director in consultation
with the GME Office or at the discretion of the DIO/designee. If a resident/fellow remains in the
training program during the appeal process, they will receive pay and benefits. If the
resident/fellow does not remain in the training program during the appeal process, they will not
receive pay but benefits will continue through the appeals process.
If a resident/fellow is terminated/dismissed, they will not receive pay, but benefits will continue
throughout the appeal process.
If an Adverse Action of termination/dismissal is rescinded at any level of appeal, the resident/fellow
will rejoin the training program. Pay will be reinstated and will be retroactive to the
termination/dismissal date.
If an Adverse Action of delayed promotion, non-renewal or termination/dismissal is rescinded at
any level of appeal, the resident/fellow will return in any remedial status in existence prior to the
Adverse Action.
Letter of Misconduct (LoM)
When the Program Director investigates an alleged Code of Conduct Violation, the Office of Graduate
Medical Education must be contacted by the Program Director as soon as it is determined that a Letter of
Misconduct may be required.
A Letter of Misconduct (LoM) is a formal written notification that states the nature of the Code of Conduct
violation and outlines the expectations of what corrective action/remediation is necessary for the
resident/fellow to successfully complete training. This status is not appealable.

120
Residents/Fellows Policies and Procedures Manual
The Letter of Misconduct must be delivered to the resident/fellow within 3 business days of the decision
of the Program Director or DIO/designee to issue the Letter of Misconduct and in a manner which requires
a signed and dated receipt of delivery to the resident/fellow and a witness signature.
If the remediation is successful and there are no further concerns in training, this status will not be
reflected on the Final Residency/Fellowship Training Summary Verification form.
The resident’s/fellow’s program file will include the following:
Documentation of (1) the meeting (s) to discuss the Code of Conduct Violation and (2) delivery of a
Letter of Misconduct to the resident/fellow
Documentation of outcome of the corrective action/remediation:
Successful remediation or
Transition to a Letter of Misconduct with Adverse Action (LoMAA)
Letter of Misconduct with Adverse Action (LoMAA)
When the Program Director investigates an alleged Code of Conduct violation, the Office of Graduate
Medical Education must be contacted by the Program Director as soon as it is determined that a Letter of
Misconduct with Adverse Action may be required.
A Letter of Misconduct with Adverse Action (LoMAA) is a formal written notification that states the nature
of the Code of Conduct violation, the Adverse Action, and where applicable, what corrective
action/remediation is necessary for the resident/fellow to successfully complete training.
Adverse Actions include:
Delayed promotion of a resident/fellow with extension of contract/appointment
Non-renewal of contract/appointment
Termination/dismissal
Adverse Actions, not the Letter of Misconduct are appealable. A resident/fellow who receives an LoMAA
must be provided with access to the appeals process.
The Letter of Misconduct with Adverse Action must be delivered to the resident/fellow within 3 business
days of the decision of the Program Director or DIO/designee to issue the Letter of Misconduct and in a
manner which requires a signed and dated receipt of delivery to the resident/fellow and a witness
signature.
The resident’s/fellow’s program file will include the following:
Documentation of (1) the meeting (s) to discuss the Code of Conduct Violation and (2) delivery of a
Letter of Misconduct with Adverse Action to the resident/fellow
Documentation of outcome of the corrective action/remediation:
o Successful remediation when the Adverse Action is extension of training or
o Non-renewal of contract/appointment or
o Termination/dismissal
The status of a resident/fellow with an LoMAA will be reflected on the Final Residency/Fellowship
Training Summary Verification form.

121
Residents/Fellows Policies and Procedures Manual
A Letter of Misconduct with an Adverse Action may not be removed from a resident’s/fellow’s official GME
file.
Appeal of Non-Academic Adverse Action
A resident/fellow is entitled to appeal an Adverse Action. At each level of appeal, the charge of the person
or committee hearing the appeal is to determine if (1) appropriate process was followed and (2) the
decision to impose an Adverse Action was made on reasonable grounds. At each level of appeal, the person
or committee hearing the appeal will either rescind or uphold the Adverse Action.
If an Adverse Action is upheld at any level of appeal, the resident/fellow must be informed about his/her
right to appeal this decision to the next level of appeal.
If an Adverse Action of extension of training is rescinded at any level of appeal, the Adverse Action will be
removed from the Letter of Misconduct. The resident/fellow must still meet any requirements for
corrective action/remediation outlined in the Letter of Misconduct. In this situation, because the Adverse
Action is removed from the LoM, this status will not be reflected on the Final Residency/Fellowship
Training Summary Verification form.
If an Adverse Action of non-renewal of contract or termination is rescinded at any level of appeal, the
Adverse Action will be removed from the Letter of Misconduct. The Program Director or DIO/designee, at
his or her discretion, may amend the Letter of Misconduct to include a required remediation/corrective
action plan or to add additional requirements to the Letter of Misconduct. In this situation, because the
Adverse Action is removed from the LoM, this status will not be reflected on the Final
Residency/Fellowship Training Summary Verification form.
If the Adverse Action is upheld upon appeal, the status of a resident/fellow with an LoMAA will be reflected
on the Final Residency/Fellowship Training Summary Verification form.
Appeals Process when the Program Director Issues a Letter of Misconduct with Adverse Action
The timelines outlined in the appeals process that follows may be adjusted if agreed upon by all parties.
Level 1: Appeal to the Department Chair, Department Designee* or GME Designee**
The resident/fellow has the right to appeal the Adverse Action. The first level of appeal is to the Department
Chair. If the Department Chair sits on the CCC, or if the Department Chair is the Program Director, or if the
Department Chair must recuse themselves due to any conflict, the resident/fellow appeal is to a
Department Designee. If an appropriate Department designee is not identified, the resident/fellow appeal
is to a GME Designee.
The resident/fellow must notify the Department Chair or Department or GME Designee of his/her request
to appeal in writing within three (3) business days of receiving the LoMAA. The Department Chair or
Department or GME Designee must acknowledge receipt of the appeal in writing to the resident/fellow.
Email is acceptable.
The resident/fellow and the Program Director must submit any documents they wish to be considered for
the appeal to the Office of Graduate Medical Education within five (5) business days of the appeal request.

122
Residents/Fellows Policies and Procedures Manual
The Department Chair or the Department or GME Designee must meet with the resident/fellow and any
additional sources (i.e., the Program Director, other faculty, staff, etc.) as they deem appropriate within ten
(10) business days of receiving the documents. The resident/fellow will be given an opportunity to provide
input at his/her meeting with the Department Chair or Department or GME Designee prior to any decision
being made.
The Department Chair or the Department or GME Designee must reach a decision regarding the appeal
and must deliver said decision in writing to the resident/fellow and the Program Director within three (3)
business days of concluding the review. The decision must be delivered in a manner which requires a
signed and dated receipt of delivery to the resident/fellow.
The resident/fellow must sign and date the written decision to acknowledge receipt of said document
within two (2) business days and deliver the signed copy to the Department Chair or Department or GME
Designee and to the Office of Graduate Medical Education. If the resident/fellow fails to do so, it will be so
noted in resident’s/fellow’s file.
Level 2: Appeal to the Associate Dean for Graduate Medical Education/Designee**
The resident/fellow has the right to appeal the decision of the Department Chair or Department or GME
designee. The second and final level of appeal is to the Associate Dean for Graduate Medical Education. If
the Associate Dean for Graduate Medical Education must recuse themselves from the appeal, the appeal
will be to a GME Designee. The Associate Dean for Graduate Medical Education or Designee will convene
an ad hoc committee to hear the appeal. The ad hoc committee is advisory to the Associate Dean for
Graduate Medical Education or GME Designee.
The resident/fellow must notify the Associate Dean for Graduate Medical Education or the GME Designee
of his/her request to appeal in writing within three (3) business days of receiving the written decision of
the Department Chair or Department or GME Designee. The Associate Dean for Graduate Medical Education
or GME Designee must acknowledge receipt of the appeal in writing to the resident/fellow. Email is
acceptable.
The resident/fellow and the Department Chair or Department or GME Designee from level 1 of the appeal
must submit documents they wish to be considered for the appeal to the Office of Graduate Medical
Education within five (5) business days of the appeal request.
The Associate Dean for Graduate Medical Education or GME Designee and the members of the ad hoc
committee must meet with the resident/fellow and any additional sources (i.e., the Program Director, other
faculty, staff, etc.) as they deem appropriate within ten (10) business days of receiving the documents. The
resident/fellow will be given the opportunity to provide input at their meeting with the ad hoc committee
and Associate Dean for Graduate Medical Education or GME Designee prior to any decision and/or
recommendation being made.
The Associate Dean for Graduate Medical Education or GME Designee must reach a decision regarding the
appeal and must deliver said decision in writing to the resident/fellow and the Program Director within
three (3) business days of concluding the review. The decision must be delivered in a manner which
requires a signed and dated receipt of delivery to the resident/fellow.

123
Residents/Fellows Policies and Procedures Manual
The resident/fellow must sign and date the written decision to acknowledge receipt of said document
within 2 business days and deliver the signed copy to the Associate Dean for Graduate Medical Education
or GME Designee and to the Office of Graduate Medical Education. If the resident/fellow fails to do so, it
will be so noted in the resident’s/fellow’s program file.
*The Department Designee will be a faculty member of the resident’s/fellow’s Department. This
faculty member may not be a member of the Clinical Competency Committee of the residency or
fellowship program, nor may they be the advisor assigned to the resident/fellow. This faculty
member cannot have had any prior involvement with the resident’s/fellow’s situation that led to
the contemplated Letter of Misconduct with Adverse Action unless this requirement is not possible.
The Department Designee will be selected by the Designated Institutional Official (DIO).
** The GME designee will be a voting member of the GMEC. This individual cannot be faculty in the
resident’s/fellow’s training program, nor can they have any prior involvement with the
resident’s/fellow’s situation that led to the contemplated Letter of Misconduct with Adverse Action
unless this requirement is not possible. The GME Designee will be selected by the Designated
Institutional Official (DIO).
The Dean of the School of Medicine will be notified of the final decisions of the Associate Dean for
Graduate Medical Education or GME Designee regarding Adverse Actions. The Dean of the School
of Medicine will also be notified if there is no appeal of an Adverse Action.
Appeals Process when the DIO/Designee Issues a Letter of Misconduct with Adverse Action
The timelines outlined in the appeals process that follows may be adjusted if agreed upon by all parties.
Appeal to the Associate Dean for Graduate Medical Education/Designee**
The resident/fellow has the right to appeal the Adverse Action. The appeal is to the Associate Dean for
Graduate Medical Education. If the Associate Dean for Graduate Medical Education must recuse themselves
from the appeal, the appeal will be to a GME Designee. The Associate Dean for Graduate Medical Education
or Designee will convene an ad hoc committee to hear the appeal. The ad hoc committee is advisory to the
Associate Dean for Graduate Medical Education or GME Designee.
The resident/fellow must notify the Associate Dean for Graduate Medical Education or the GME Designee
of his/her request to appeal in writing within three (3) business days of receiving the Letter of Misconduct
with Adverse Action. The Associate Dean for Graduate Medical Education or GME Designee must
acknowledge receipt of the appeal in writing to the resident/fellow. Email is acceptable.
The resident/fellow and the DIO/designee must submit documents they wish to be considered for the
appeal to the Office of Graduate Medical Education within five (5) business days of the appeal request.
The Associate Dean for Graduate Medical Education or GME Designee and the members of the ad hoc
committee must meet with the resident/fellow and any additional sources (i.e., the Program Director, other
faculty, staff, etc.) as they deem appropriate within ten (10) business days of receiving the documents. The
resident/fellow will be given the opportunity to provide input at his/her meeting with the ad hoc
committee and Associate Dean for Graduate Medical Education or GME Designee prior to any decision
and/or recommendation being made.

124
Residents/Fellows Policies and Procedures Manual
The Associate Dean for Graduate Medical Education or GME Designee must reach a decision regarding the
appeal and must deliver said decision in writing to the resident/fellow and the Program Director within
three (3) business days of concluding the review. The decision must be delivered in a manner which
requires a signed and dated receipt of delivery to the resident/fellow.
The resident/fellow must sign and date the written decision to acknowledge receipt of said document
within 2 business days and deliver the signed copy to the Associate Dean for Graduate Medical Education
or GME Designee and to the Office of Graduate Medical Education. If the resident/fellow fails to do so, it
will be so noted in the resident/fellow program file.
** The GME designee will be a voting member of the GMEC. This individual cannot be faculty in the
resident’s/fellow’s training program, nor can they have any prior involvement with the
resident’s/fellow’s situation that led to the contemplated Letter of Misconduct with Adverse Action
unless this requirement is not possible. The GME Designee will be selected by the Designated
Institutional Official (DIO).
The Dean of the School of Medicine will be notified of the final decision of the Associate Dean for
Graduate Medical Education or GME Designee regarding adverse actions. The Dean of the School of
Medicine will also be notified if there is no appeal of an Adverse Action.
Revised 5/15, 3/17, 11/17 4/19, 3/21, 10/22, 10/23, 6/24, 7/24 Reviewed 4/19
125
Residents/Fellows Policies and Procedures Manual
ADMINISTRATIVE LEAVE
A resident/fellow may be placed on Administrative Leave for reasons including but not limited to the
investigation of an alleged Code of Conduct Violation (see Code of Conduct Policy), or the need for a Fit for
Duty Evaluation (see Fit for Duty/Employee Assistance Evaluation Policy). Administrative Leave is not a
sanction. It is taken in an effort to protect the safety and wellbeing of the resident/fellow, of patients, of
other individuals with whom the resident/fellow has contact, and/or of the School of Medicine and its
affiliated hospitals. Because continuous training is vital to all residency and fellowship programs, the length
of Administrative Leave can be no longer than 90 days. A resident/fellow will receive full pay and benefits
while on Administrative Leave.
The Program Director must consult with the DIO/designee regarding all cases being considered for
Administrative Leave.
If a Program Director is considering placing a resident/fellow on Administrative Leave, they will meet, if
possible, with the resident/fellow in order to gain their input before making that decision. Documentation
of that meeting (or attempt) will be placed in the resident’s/fellow’s file.
If the concern giving rise to the Administrative Leave is not substantiated or is satisfactorily resolved, the
resident/fellow will return to the program. Administrative Leave can result in an extended appointment
period (extension of training) to meet all of the requirements of the program and all of the requirements
to be eligible for board certification (see Contract Extension Due to Leave Guidelines Policy). If this occurs,
a resident/fellow may choose to use vacation time to offset any appointment extension that results from
the Administrative Leave. If the resident’s/fellow’s time away from the program due to Administrative
Leave results in an extension of training, this leave may be reported only as approved leave.
If an alleged Code of Conduct Violation is the reason for placing the resident/fellow on Administrative
Leave and the allegation is substantiated (see the Academic Deficiencies and Code of Conduct
Violations/Non-Academic Deficiencies Review Process Policy).
If a Fit for Duty/EAP Evaluation is the reason for placing the resident/fellow on Administrative Leave see
the Fit for Duty/Employee Assistance Evaluations Policy.
If an investigation into an allegation including those involving an alleged Code of Conduct Violation extends
beyond the 90 days of Administrative Leave, the Program Director and the DIO/designee will make a
determination regarding the resident’s/fellow’s status in their training program. Such a determination will
be based on both the preponderance of evidence (whether it is more likely than not that a violation
occurred) and on an analysis of the requirement of continuous training that is vital to all residency and
fellowship programs as well as any concerns regarding the safety and wellbeing of the resident/fellow, of
patients, of other individuals with whom the resident/fellow has contact, and/or of the School of Medicine
and its affiliated hospitals. The Program Director and the DIO/designee may take action which may include
but is not limited to reinstatement, extension of training, non-renewal or termination (see the Academic
Deficiencies and Code of Conduct Violations/Non-Academic Deficiencies Review Procedures Policy.).
Revised 3/16, 3/17, 4/19, 3/21
Reviewed 2/23

126
Residents/Fellows Policies and Procedures Manual
SECTION V: EMPLOYMENT GUIDELINES
AND PROCEDURES
127
Residents/Fellows Policies and Procedures Manual
AFFIRMATIVE ACTION, NON-DISCRIMINATION, AND EQUAL OPPORTUNITY
It is the policy of the University of Connecticut School of Medicine to provide equal employment
opportunities for all residents/fellows, employees, and applicants, in compliance with the UConn Health
affirmative action policy and is as follows:
To recruit, train, hire, transfer, and promote in all job classifications without regard to race, color,
religion, age, sex, national origin, physical or mental disability, veteran status, sexual orientation or
marital status.
To base decisions on employment in accordance with the principles of equal employment
opportunity.
To make promotion decisions in accordance with the principles of equal employment opportunity.
To provide that all other personnel actions and terms and conditions of employment will be
administered without regard to race, color, religion, age, sex, physical or mental disability, national
origin, sexual orientation, marital status, or any other characteristics protected by state and/or
federal law.
For a more detailed description of this policy, please see the following:
http://health.uconn.edu/policies/wp-content/uploads/sites/28/2015/07/policy_2002_44.pdf
Revised 8/17, 4/19
Reviewed 3/21, 2/23
128
Residents/Fellows Policies and Procedures Manual
PERSONS WITH DISABILITIES/ACCOMMODATIONS FOR DISABILITIES
The University of Connecticut School of Medicine is committed to achieving equal educational and
employment opportunity and full participation for persons with disabilities. It is the University’s policy
that no qualified person be excluded from consideration for employment, participation in any University
program or activity, be denied the benefits of any University program or activity, or otherwise be subjected
to discrimination with regard to any University program or activity. This policy derives from the
University’s commitment to nondiscrimination for all persons in employment, academic programs, and
access to facilities, programs, activities, and services. See UConn Health Policy.
State and Federal laws prohibit discrimination against individuals with disabilities. Discrimination
includes failing to provide reasonable accommodation, consistent with state and federal law, to persons
with disabilities.
If a resident/fellow thinks that they might need a reasonable accommodation, the resident/fellow should
contact Lauren Hurley in Human Resources at UConn Health.
Phone: 860-679-8004
Fax: 860-679-4660
Email: lhurley@uchc.edu
Website: https://health.uconn.edu/human-resources/services/americans-with-disabilities-act-
compliance-and-accommodations/
Mailing Address:
ADA Accommodations Case Manager
UConn Health
P.O. Box 4035
Farmington, CT 06030-4035
Physical Address:
16 Munson Rd., 5
th
Floor
Farmington, CT 06030-4035
UConn Health Internal Mail: MC 4035
The Human Resources website has more detailed information, including links to information regarding the
reasonable accommodation process and accommodation request forms:
https://health.uconn.edu/human-resources/services/americans-with-disabilities-act-compliance-and-
accommodations/
Revised 4/16, 3/17, 7/17, 9/18, 3/21, 11/22, 2/23, 3/23, 11/23
Reviewed 4/19
129
Residents/Fellows Policies and Procedures Manual
RELIGIOUS ACCOMMODATIONS
The University of Connecticut prohibits discrimination, harassment, and retaliation on the basis of religion.
For more information, refer to the University Policy Against Discrimination, Harassment and Related
Interpersonal Violence and Non-retaliation Policy.
The University of Connecticut School of Medicine is committed to providing welcoming and inclusive
learning and workplace environments. As part of this commitment, the residency/fellowship programs
will make good faith efforts to provide reasonable religious accommodations to residents/fellows whose
sincerely held religious practices or beliefs conflict with a University policy, procedure, or other academic
or employment requirement, unless such an accommodation would create an undue hardship.
The University defines a religious practice or belief as a sincerely held practice or observance that includes
moral or ethical beliefs as to what is right and wrong, most commonly in the context of the cause, nature
and purpose of the universe. Religion includes not only traditional, organized religions, but also religious
beliefs that are new, uncommon, not part of a formal religious institution or sect, or only subscribed to by
a small number of people. Social, political, or economic philosophies, as well as mere personal preferences,
are not considered to be religious beliefs.
If a resident/fellow thinks that they might need a religious accommodation, the resident/fellow should
make the request directly to the program director with as much reasonable notice as possible. The Program
Director, in consultation with the GME Office, will evaluate the request in order to determine if it will be
granted. This determination will consider whether or not the requested accommodation will pose an undue
hardship for the program and/or interfere with the resident’s/fellow’s essential job functions or
educational requirements.
In keeping with the School of Medicine’s commitment to building and maintaining a welcoming and
inclusive work environment, the residency/fellowship program and the GME Office will consider religious
accommodations requests by residents/fellows based on the totality of the circumstances.
Created 3/21
Reviewed 2/23
130
Residents/Fellows Policies and Procedures Manual
LEAVE POLICY/GUIDELINES
Residents/fellows are entitled to several different types of leave. Taking any leave (especially when
multiple leaves or absences occur in the same contract year) may extend the time necessary to complete
the program requirements for graduation as well as for board eligibility (see Contract Extension Due to
Leave Guidelines Policy). Residents/fellows are responsible for understanding their Residency Review
Committee/Program requirements for program completion as well as their Board requirements regarding
Board eligibility, specifically as it relates to time away from their program.
All sick and vacation leave is designed to meet the average amount of time allowed away from any of the
programs sponsored by the UConn SOM. All residents/fellows must abide by these policies as well as any
and all policies of their specific specialty Board. To the extent there is any conflict between these policies
and the policies of a specific specialty board, the stricter policy must be adhered to.
Vacation Leave
Sick Leave
Leave Policy Overview
GME One-Time Leave Policy
CT Family and Medical Leave (CTPFML), Federal Family and Medical Leave (FMLA) and CT Paid
Family and Medical Leave (CTPFML)
o Medical Leave
o Other Non-Medical CTFMLA and FMLA Leaves and CT Paid FMLA Leave
o Military Leave
Emergency Leave
Bereavement Leave
Personal Leave
Contract Extension Due to Leave Guidelines
All leaves, regardless of category, needs to be reported by the resident to their Program Director and the
CAHC. Residents/fellows may not participate in any program related clinical or education activities while
on any type of leave without the express permission of his/her Program Director in consultation with the
GME Office.
Revised 2/16, 3/17, 5/17, 8/17, 10/18, 4/19, 12/21, 5/22
Reviewed 3/21, 2/23
131
Residents/Fellows Policies and Procedures Manual
VACATION LEAVE
The UConn SOM provides residents/fellows with four weeks paid vacation per contract year. (A week is
equal to 5 weekdays and 2 weekend days). Each resident/fellow is responsible for knowing and following
their program’s policy on paid vacation. The Program Director or designee schedules vacation leave to
ensure adequate coverage of educational and clinical responsibilities and, therefore, requests may be
denied or approved, and vacations may need to be changed at times. Vacation leave cannot be carried over
into a new academic year nor can vacation leave be borrowed from a subsequent year of training.
Use of available vacation time for Connecticut Paid Family Medical Leave (CTPFML) and GME leaves is
required to be used prior to receiving any paid leave benefits under CAHC’s private plan. Employees can
reserve two weeks of vacation time for future use if available at the time of the leave. A resident/fellow
may choose to use the reserved vacation as leave to receive full pay under family leave but must do so in
writing sent to [email protected].
If a resident/fellow needs to extend their training for any reason, vacation time will be determined by the
Program Director in consultation with the GME Office prior to their extension (see Contract Extension Due
to Leave Guidelines Policy).
Revised 3/16, 3/17, 5/17, 4/19, 3/21, 12/21, 1/23, 8/23, 10/23, 6/24
132
Residents/Fellows Policies and Procedures Manual
SICK LEAVE
Residents/fellows receive up to 10 working days per contract year of paid sick leave. Sick time may not be
carried over into the next contract year. In the event of serious injury or prolonged illness, or injury,
residents/fellows may be eligible for a paid or unpaid leave of absence as set forth in the GME One-Time
Leave Bank Policy (see GME One-Time Leave Bank Policy, CT Family and Medical Leave (CTFMLA), Federal
Family and Medical Leave (FMLA) and CT Paid Family and Medical Leave (CTPFML) Policy, and the Medical
Leave Policy).
CAHC will require a treating health provider’s letter for any absence due to illness or injury, depending on
the absence’s nature and length of time. A treating health provider’s letter is mandatory after 3 consecutive
workdays off for illness or injury stating that the resident/fellow may return to work. A treating health
provider’s letter is also mandatory in order for a resident/fellow to work following a hospital visit (ED or
inpatient). Every program has its own policy on handling sick days that may add requirements to this
policy. Residents/fellows are required to know and follow their specific program policy. At a minimum, a
resident/fellow must notify their program office and appropriate supervising physician as soon as known,
but clearly before their shift begins, if absent due to illness or injury.
Use of available sick time for Connecticut Paid Family Medical Leave (CTPFML) and GME leaves is required
prior to receiving any paid leave benefits under CAHC’s private plan.
Taking any leave (especially when multiple leaves or absences occur in the same contract year) may extend
the time necessary to complete the program requirements for graduation as well as for Board eligibility
(see Contract Extension Due to Leave Guidelines Policy). Residents/Fellows are responsible for
understanding their Residency Review Committee/Program requirements for program completion as well
as their Board requirements regarding Board eligibility, specifically as it relates to time away from their
program.
Revised 3/16, 3/17, 5/17, 4/19, 12/21, 1/23, 8/23, 6/24
Reviewed 3/21

133
Residents/Fellows Policies and Procedures Manual
LEAVE POLICY OVERVIEW
ALL AVAILABLE LEAVES WILL RUN CONCURRENTLY AT ALL TIMES
One-Time GME Leave Benefit
Beginning on the first day of employment, all residents/fellows have up to 6 weeks of paid medical, family
or caregiver leave available that may be used for qualifying reasons consistent with Connecticut law. This
one-time leave will be paid at 100% of pay for both Medical and Family Leave reasons. Vacation and sick
time for medical leaves, and vacation time for family leaves is required to be used toward the leave.
Employees can reserve two weeks of vacation time for future use if available at the time of leave.
If the first leave required is longer than 6 weeks or if a second leave is required during residency, the leave
coverage available will fall under the CT Paid Leave Law. If the criteria for CT Paid Leave is not met and a
leave greater than 6 weeks is required, the remaining leave will be unpaid.
CT Paid Leave Benefit
All leaves of absence will be paid per Capital Area Health Consortium’s (CAHC) CT Paid Leave Private Plan.
To be eligible for CT Paid Leave, residents/fellows must have been employed by CAHC for at least 3 months.
If employed in CT before joining CAHC, residents/fellows may be eligible for the CT Paid Leave benefit at
an earlier time if the eligibility criteria are met.
The rates of pay are as follows:
Medical/Maternity Leave:
• Paid at 100% of pay for the “medical leave” period that the resident/fellow’s health provider
indicates they are unable to work for health reasons (for maternity leave, the health provider will
authorize 6 weeks following a non-surgical delivery and 8 weeks following a surgical delivery). An
employee may be granted an extension of “medical leave” by submitting updated medical
documentation from their health care provider indicating the medical reason the extension is
required.
• Additional leave time taken past the “medical leave” period will be considered “family leave” and
will be paid at the approved State rate (see below for further details).
Family/Non-Medical Leave:
• Paid at the State maximum benefit rate. On 1/1/24, the rate increased to $941.40/week or
$1,882.80/bi-weekly.
Leave Duration:
Medical and Family Leave under the CT Paid Family and Medical Leave Act is for up to 12 weeks of pay in
a 12-month period. An additional 2 weeks of paid leave time may be provided for pregnancy incapacities.
A maximum of 12 total days of paid leave compensation may be paid in a single calendar year for leave
due to the Covered Employee being the victim of family violence.
Taxability of Paid Leave Income

134
Residents/Fellows Policies and Procedures Manual
• FICA and FLI taxes are not required on paid leave income and will not be withheld from leave pay,
resulting in a higher net leave pay. CT Paid Leave will continue to withhold Federal and State tax
since leave pay is taxable under these jurisdictions.
Accrued Time Requirement
For Medical Leaves, vacation and sick time is required to be used, and for Family Leaves, vacation time
is required to be used prior to receiving any paid leave benefits under CAHC’s private plan. Employees can
reserve two weeks of vacation time for future use if available at the time of leave.
Qualifying Leave Reasons Under CT Law
• Medical Leave – to care for your own serious health condition.
• Non-Medical/Family Leaves – to attend to family responsibilities.
o Parental Leave to bond with a newborn child or one that has joined the family through
adoption or foster care.
o Maternity Leave Post Medical Period to bond with a newborn child once the medical leave
period has ended.
o Caregiver Leave to care for a covered family member with a serious health condition.
o Family Violence Leave to attend to specific issues associated with family violence.
o Military Exigency or Military Caregiver Leave to attend to specific issues associated with
a covered family member’s deployment, care for an active duty injured service member, or
to care for a veteran with a serious health condition.
Leave Paperwork
All leaves of absence require specific paperwork verifying the need for leave and its beginning and ending
dates. Early submission of this paperwork will help CAHC to provide the resident/fellow with continuous
pay so please submit as soon as possible. Please contact CAHC to obtain leave paperwork. Please be advised
that all leave paperwork including return to work notes for medical leaves must be returned to CAHC and
not to the program or the GME office.
Requesting Leave
In the case of foreseeable leaves, residents/fellows must provide at least 30 days’ notice to CAHC and their
program before the leave begins. If the leave is unforeseeable, you must provide notice to CAHC and your
program as soon as practicable.
Extending a Medical Leave
Residents/fellows may extend a medical leave for the same condition by submitting updated medical
documentation from their health care provider indicating the reason for the extension and an estimated
return to work date. A return-to-work note cannot extend medical leave. An extension must be
provided by the health provider stating the medical need.
If the extension is for a new medical issue or condition, a new CTPFML application must be submitted.
Return from Leave
135
Residents/Fellows Policies and Procedures Manual
When possible, a resident/fellow should provide their Program Director and CAHC with at least 2 weeks’
advance notice of the date they intend to return to training.
A return to work note from the resident/fellow’s health provider stating that they are able to resume work
duties is required for all Medical Leaves of absence of 3 days or more or following any hospital visit (ED
or inpatient) and must be submitted to CAHC before the resident/fellow’s return to work.
If a resident/fellow is unable to return following a leave, they must contact CAHC, their Program Director,
and the GME office as soon as possible.
Time Entry (MyEvaluations) When on Leave
Residents/fellows are not required to log time when on approved leave. They may willingly enter time to
keep up with it; otherwise, residents/fellows will need to attend to it immediately upon return before the
next closest pay period.
o For Medical/Maternity Leaves – enter in the Sick/Med LV category
o For Family/Non-Medical Leaves – enter in the NonMedical LV category
Time Away from Training
Taking any leave may extend the time necessary to complete the program requirements for graduation as
well as Board eligibility (see Contract Extension Due to Leave Guidelines Policy). Residents/fellows are
responsible for understanding their Residency Review Committee/Program requirements for program
completion as well as their Board requirements regarding Board eligibility, specifically as it relates to time
away from their program. If more than 12 weeks of leave time is needed, the time will be unpaid and time
off must be approved by your Program Director and the GME office.
Revised 1/23, 8/23, 6/24
136
Residents/Fellows Policies and Procedures Manual
GME ONE-TIME LEAVE BANK POLICY
Beginning on the resident’s/fellow’s first day of employment, each resident/fellow will have up to six (6)
weeks of paid medical, parental and caregiver leave at 100% of salary to be used for qualifying reasons
that are consistent with Connecticut law (see CT Family and Medical Leave (CTFMLA), Federal Family and
Medical Leave (FMLA) and CT Paid Family and Medical Leave (CTPFML) Policy). The requirements for the
use of this GME leave are as follows:
• The GME leave may be used one-time during the resident’s/fellow’s program, but once any leave
time is used, it exhausts and does not renew.
• The GME leave shall run concurrently with other leaves of absence and time off for which the
resident/fellow may qualify under Connecticut and Federal law, these policies and the policies
governing the resident’s/fellow’s program. This includes leaves of absence under the CT Family and
Medical Leave, the CT Paid Family and Medical Leave and the Federal Family and Medical Leave and
the vacation and sick leave policies applicable to the resident’s/fellow’s program. Please see the
specific policies for details regarding the CT Family and Medical Leave, Federal Family and Medical
Leave and CT Paid Family and Medical Leave and policies governing the use of vacation and sick
time (see CT Family and Medical Leave (CTFMLA), Federal Family and Medical Leave (FMLA) and
CT Paid Family and Medical Leave (CTPFML) Policy, Vacation Leave Policy, and Sick Leave Policy).
Also, please see your specific program policy governing vacation and sick time.
• The medical certification requirements applicable to the CTFMLA and Federal FMLA leaves will
apply to GME leave.
Timing of GME Leave During Training
1.) If the need for leave occurs before the resident/fellow is eligible for CT Paid Family and Medical
Leave (less than 3 months of employment)*, the use of the GME leave will be as follows:
• Residents/Fellows are required to use vacation and sick time for medical leaves and vacation
time for family leaves at the beginning of the leave (while reserving 2 weeks of vacation time for
further use if available at the time of leave) provided under CAHC’s policies and their specific
program policies during the GME leave. Once vacation and sick time (for medical leave use only)
is exhausted, CAHC will provide 100% of pay for up to a combined total of 6 weeks (including
time used) one-time during residency. Any additional leave required will be unpaid unless the
resident becomes eligible for CT Paid Leave benefits.*
*GME leave time for residents/fellows with less than 3 months of employment does not qualify as
job-protected leave under the CT Family and Medical Leave Act. However, residents/fellows may
qualify for CT Paid Leave as early as their date of hire if they had been working in CT and they meet
the eligibility criteria.
2.) For residents/fellows who have been employed for 3 months or more and are eligible for CT Family
and Medical Leave, the use of the GME leave will be as follows:
• Residents/Fellows are required to use vacation and sick time for medical leaves and vacation
time for family leaves prior to receiving any paid leave benefits under CAHC’s private plan (while
137
Residents/Fellows Policies and Procedures Manual
reserving 2 weeks of vacation time for future use if available at the time of leave) provided under
CAHC’s policies and their specific program policies during the GME leave.
Residents/fellows may qualify for CT Paid Leave as early as their date of hire if they had been
working in CT and meet the eligibility criteria. For family leaves (including parental leave), once
vacation is exhausted, CAHC will supplement the difference between the CT Paid Family Leave
benefit rate and 100% of pay for up to 6 weeks (including vacation time used) one-time during
residency. If additional family leave is required after the 6 week period, the CT Family and
Medical Leave Act will apply and the leave will be paid at the State’s benefit rate; which is capped
at 60 times the minimum wage rate (see Other Non-Medical Leave policy).
• During the GME leave, health and disability insurance benefits will continue for the
resident/fellow and their dependents at the same level as before the GME leave began.
Requests for GME leave should be directed to CAHC at [email protected]. Upon request, CAHC will
provide the necessary forms for completion.
To the extent applicable, any family/parental leave, GME leave, CT Family and Medical Leave, Federal
Family and Medical Leave, and CT Paid Leave will run concurrently.
Revised 1/23, 8/23, 10/23

138
Residents/Fellows Policies and Procedures Manual
CT FAMILY AND MEDICAL LEAVES OF ABSENCE (CTFMLA), FEDERAL FAMILY AND
MEDICAL LEAVE (FMLA) AND CT PAID FAMILY AND MEDICAL LEAVES OF ABSENCE
(CTPFML)
Overview
Under the Connecticut Family and Medical Leave Act (“CTFMLA”) and the Federal Family and Medical
Leave Act (“FMLA”), residents/fellows may be eligible for family and medical leaves of absence for
specified reasons. Residents/Fellows may also be eligible for paid leave benefits after using available
vacation and sick leave as described below.
Under CTPFMLA, residents/fellows who have worked for CAHC for at least 3 months are eligible for up to
12 weeks of leave in a 12-month period, up to 14 weeks for incapacitation during pregnancy, up to 12 days
for family violence leave and up to 26 weeks for military caregiver leave. Residents/fellows may qualify for
CTPFMLA as early as their hire date if they have been working in CT and meet the eligibility criteria.
Under FMLA, a resident/fellow who has worked for at least 12 months and for at least 1,250 hours during
the preceding 12-month period may take up to 12 weeks of unpaid leave in a 12-month period, except that
an eligible resident/fellow may take up to 26 weeks of leave to care for a covered service member, as
explained below.
A resident/fellow who is eligible for leave under only one law will receive benefits in accordance with that
law only. However, if the resident’s/fellow’s leave qualifies for CTFMLA, CTPFML, and FMLA, the leave will
count against their entitlement under State and Federal laws and will run concurrently. If the
resident/fellow is eligible for GME leave, said leave will run concurrently with the leaves provided in this
policy (see GME One-Time Leave Bank Policy). If the resident/fellow and their spouse are both employed
by CAHC, special rules may apply, and their combined leave may be limited.
Calculation of 12-Month Period
The 12-month period is measured backward from the date an employee uses any family and medical leave.
Under this “rolling” 12-month period, each time an employee takes family and medical leave, the remaining
leave entitlement would be the balance of the 12 weeks that has not been used during the immediately
preceding 12 months. Military caregiver leaves are measured based on a 12-month period measured
forward from the employee’s first date of leave.
Qualifying Reasons for CTFMLA, CTPFML, and FMLA
Resident’s/Fellow’s may apply for a family and medical leave under the CTFMLA, CTPFML, and FMLA for
the following reasons:
1. The birth of a son or daughter of the employee, or to bond with a newborn or newly placed child via
adoption or foster care, including the time needed to process adoption or foster care placement;
2. Under the FMLA, to care for a parent, spouse, or child who is under 18 with a serious health
condition, or under 18 with a disability;
3. Under the CTFMLA, to care for a family member of the employee if the family member has a serious
health condition.
139
Residents/Fellows Policies and Procedures Manual
• Family member is defined as a parent, spouse, son or daughter of any age, sibling, grandparent,
grandchild, or an individual related to the employee by blood or affinity whose close association
to the employee shows to be the equivalent of those family relationships.
• Related by affinity means any person with whom the employee has a significant personal bond
that is like one of the family relationships noted above, regardless of biological or legal
relationship.
4. To care for the employee’s own serious health condition, which under the CTFMLA, CTPFML
includes the employee serving as an organ or bone marrow donor and incapacity due to pregnancy.
5. Under the CTFMLA, CTPFML if the employee is experiencing family violence, the employee may
apply to take up to 12 days of leave.
6. For any qualifying exigency arising out of the fact that the spouse, son, daughter, or parent of the
employee is on active duty or has been notified of an impending call or order to active duty in the
armed forces and to care for a military family member who experienced a serious injury or illness.
7. A serious health condition is defined by law and means an illness, injury, impairment, or physical or
mental condition that involves inpatient care in a hospital, hospice, or residential medical care
facility, or continuing treatment by a health care provider.
Please see (Medical Leave Policy), (Other Non-Medical Leave) and (Military Leave Policy) for specific
requirements governing eligibility.
Procedures
All requests for leave should be directed to the CAHC by emailing cah[email protected]. CAHC will provide
the resident/fellow with all necessary forms requiring completion.
Eligibility for Paid Leave (CTPFML)
CT Paid Family and Medical Leaves of Absence (CTPFML) is available to eligible residents/fellows (those
who are currently employed or have been employed by CAHC within the last 12 weeks and have earned
wages of at least $2,325 in the highest earning quarter of the first four of the five most recently completed
quarters) who require time off from work duties to fulfill covered family and medical events provided for
in the CTFMLA, which are outlined above and described more fully below in the Medical and Non-Medical
Leave policies. For military service personnel or spouses of military service personnel in the military or
military reserves (see Military Leave Policy). All decisions regarding paid leave are in accordance with
CAHC’s private plan.
Use of Accrued Time
For Medical Leaves, vacation and sick time are required to be used and for Family Leaves, vacation time
is required to be used prior to receiving any paid leave benefits under CAHC’s private plan (while
reserving 2 weeks of vacation time for future use if available at the time of leave).
To the extent applicable, any CT Family and Medical Leave, Federal Family and Medical Leave, CT
Paid Leave, and GME Leave will run concurrently.
Revised, 5/22, 1/23, 8/23, 10/23
Created 12/21
140
Residents/Fellows Policies and Procedures Manual
MEDICAL LEAVE
Residents/Fellows who have been employed for 3 months or more and require time off from their work
duties to care for their own serious health condition (emergent or non-emergent) as defined under
Connecticut law are eligible for CT Family and Medical Leave (CTFMLA) and those employed for 12 months
or more are eligible for Federal Family and Medical Leave (FMLA). Both of these leaves are unpaid (see CT
Family and Medical Leave of Absence (CTFMLA), Federal Family and Medical Leave (FMLA), and CT Paid
Family and Medical Leaves of Absence (CTPFML) Policies).
Paid Medical Leave
Residents/Fellows are eligible for paid GME leave and CT Paid Family and Medical Leave (CTPFML)
benefits administered by CAHC’s private plan once eligibility requirements are met (see GME One-Time
Leave Policy, CT Family and Medical Leave of Absence (CTFMLA), Federal Family and Medical Leave
(FMLA), and CT Paid Family and Medical Leaves of Absence (CTPFML) Policies).
Medical leave eligibility requires a treating health provider’s certification verifying the need for medical
leave and its beginning and expected end dates. Residents/fellows are required to use their available
vacation time and sick time for both GME and CTPFML prior to receiving any paid leave benefits under
CAHC’s private plan. Employees can reserve two weeks of vacation time for future use if available at the
time of the leave). Four weeks of vacation and 10 working days of sick time is available to residents/fellows
on the first day of employment.
GME Leave
GME leave time is available on the first day of employment. Residents/fellows who require time off to care
for their own serious health condition as defined under Connecticut law are eligible for GME leave benefits
for up to 6 weeks of pay at 100% of salary once during residency/fellowship. If additional medical leave
time is required after GME leave is exhausted but before eligible for CTPFML, leave will be unpaid (see GME
One-Time Leave Bank Policy).
CTPMFL Leave
CTPMFL leave time is available after 3 months of employment in most cases. Residents/fellows who
require time off to care for their own serious health condition as defined under Connecticut law are eligible
for CTPMFL paid benefits after meeting eligibility requirements. For medical leaves, CAHC’s private plan
pays 100% of salary. Maternity leaves extending past the treating health provider’s statement will be
considered family leave and paid at the State’s benefit rate, which is capped at 60 times the minimum wage
rate for the remaining period of absence (not to exceed 12 weeks or 84 days in a twelve-month period). A
resident/fellow may elect to use their reserved vacation time to supplement the State’s rate cap and receive
additional pay if a request is submitted to CAHC in writing. Leaves in most cases, that extend past 12 weeks,
will be unpaid and will be classified as “other leave” (see CT Family and Medical Leave of Absence
(CTFMLA), Federal Family and Medical Leave (FMLA), and CT Paid Family and Medical Leaves of Absence
(CTPFML) Policies).
To the extent applicable, any medical leave, GME leave, CT Family Medical Leave, Federal Family
and Medical Leave, and CT Paid Leave will run concurrently.
141
Residents/Fellows Policies and Procedures Manual
Maternity Leave
Maternity Leaves are considered Medical Leaves and are available to all eligible residents/fellows who are
unable to work due to pregnancy related conditions. Employees eligible for CT Paid Leave are eligible for
an additional 2 weeks of leave and paid leave benefits, up to a total of 14 weeks or 98 days, if incapacitated
by pregnancy and supported by a treating health provider’s certification. All available leaves will run
concurrently.
The resident/fellow may be eligible for Long Term Disability (LTD) benefits for medical/maternity leaves
if requiring absence of 90 days or more. The Capital Area Health Consortium can provide information
regarding this process. CAHC and the Program Director should be notified as soon as possible if there is a
chance the resident/fellow might apply for such benefits.
A treating health provider’s certification verifying the need for medical/maternity leave and its beginning
and expected end dates must be submitted to the Capital Area Health Consortium with the required leave
forms. Residents/fellows should provide at least 30 days advance notice of the need for leave, when the
leave is foreseeable. When not foreseeable, a resident/fellow must notify CAHC as soon as practicable, and
certainly within two (2) business days of learning of the need for leave, except in extraordinary
circumstances. Notice of the need for leave should be provided to [email protected]. It is critical and
required that the resident/fellow also notify their Program Director as soon as it is known that the
resident/fellow needs a leave of absence.
When possible, the resident/fellow is required to provide their Program Director and the Capital Area
Health Consortium with at least two weeks’ advanced notice of the date the resident/fellow intends to
return to training. When a resident/fellow returns from leave, the Program Director in consultation with
the GME Office will determine the resident/fellow’s status in the program specifically as it relates to an
extension of training and whether the resident/fellow may return to their previous level of training (see
Contract Extension Due to Leave Guidelines Policy).
A return-to-work note from the resident/fellow’s health provider stating that they can resume work duties
is required for all medical leave absences and must be submitted to CAHC before return to work. A return-
to-work note is not a substitute for a provider’s certification of a medical time extension. If the return date
is later than the previous certification, a new certification is required stating a specific need for the
extended absence. A return-to-work note is not required for maternity leaves that have been extended for
bonding purposes. If a resident/fellow fails to report to work promptly at the end of the medical/maternity
leave, their appointment with the UConn SOM and their employment with CAHC may be terminated.
If a resident/fellow is unable to return to training after 12 weeks of medical leave (14 weeks if
incapacitated by pregnancy), they must contact CAHC, their Program Director, and the Office of Graduate
Medical Education as soon as possible.
The status of a resident/fellow who is unable to return to training after 12 weeks of medical leave (14
weeks if incapacitated by pregnancy), leave will be determined by the Program Director in consultation
with the GME Office. The position of the resident/fellow may or may not be held.

142
Residents/Fellows Policies and Procedures Manual
Taking any leave may extend the time necessary to complete the program requirements for graduation as
well as Board eligibility (see Contract Extension Due to Leave Guidelines Policy). Residents/fellows are
responsible for understanding their Residency Review Committee/Program requirements for program
completion as well as their Board requirements regarding Board eligibility, specifically as it relates to time
away from their program.
Revised 4/19, 10/20, 5/21, 12/21, 5/22, 1/23, 8/23, 10/23, 6/24
Reviewed 3/21
143
Residents/Fellows Policies and Procedures Manual
OTHER NON-MEDICAL LEAVE
Family Leaves Including Parental Leave
Residents/Fellows who have been employed for 3 months or more and need to care for a family member
with a serious health condition, bond with a newborn child or one that has joined the family through
adoption or foster care, for exigent circumstances, or for family violence as defined under Connecticut law
are eligible for CT Family and Medical Leave (CTFMLA) and those employed for 12 months or more are
eligible for Federal Family and Medical Leave (FMLA). Both of these leaves are unpaid (see CT Family and
Medical Leaves of Absence (CTFMLA), Federal Family and Medical Leave (FMLA) and CT Paid Family and
Medical Leaves of Absence (CTPFML) Policy).
Paid Family Leave
Residents/fellows are eligible for paid GME leave and CT Paid Family Medical Leave (CTFML) benefits
administered by CAHC’s private plan once eligibility requirements are met (see GME One-Time Leave
Policy, CT Family and Medical Leaves of Absence (CTFMLA), Federal Family and Medical Leave (FMLA) and
CT Paid Family and Medical Leaves of Absence (CTPFML) Policy).
Family leave eligibility requires leave paperwork verifying the need for leave and its beginning and
expected end dates. Residents/fellows are required to use their available vacation time for both GME and
CTPFML prior to receiving any paid leave benefits under CAHC’s private plan (while reserving two weeks
of vacation time for future use if available at the time of the leave). Four weeks of vacation time is available
to residents/fellows on the first day of employment.
GME Leave
GME leave time is available on the first day of employment. Residents/fellows who require time off for
family leave as defined under Connecticut law are eligible for GME leave benefits for up to 6 weeks of pay
at 100% of salary once during residency. If additional medical leave time is required after GME leave is
exhausted but before eligibility criteria are met for CTPFML, leave will be unpaid (see GME One-Time Leave
Bank Policy).
CTPMFL Leave
CTPMFL leave time is available after 3 months of employment in most cases. Residents/fellows who
require time off for family leaves as defined under Connecticut law are eligible for CTPMFL paid benefits
after meeting eligibility requirements. For family leaves, CAHC’s private plan pays at the State’s benefit
rate, which is 60 times the minimum wage rate for the remaining period of absence (not to exceed 12 weeks
or 84 days in a twelve-month period). A resident/fellow may elect to use reserved vacation time to
supplement the State’s rate cap and receive additional pay if a request is submitted to CAHC in writing.
Leaves in most cases, that extend past 12 weeks will be unpaid and will be classified as “Other Leave” (see
CT Family and Medical Leave of Absence (CTFMLA), Federal Family and Medical Leave (FMLA) and CT Paid
Family and Medical Leaves of Absence (CTPFML Policy).
To the extent applicable, any family/parental leave, GME leave, CT Family and Medical Leave,
Federal Family and Medical Leave, and CT Paid Leave will run concurrently.
144
Residents/Fellows Policies and Procedures Manual
The resident/fellow needing family/parental leave must submit the required paperwork to the Capital
Area Health Consortium. A resident/fellow must provide their Program Director as much notice of the
need for a family/parental leave as is practicable under the circumstances. A resident/fellow should
provide at least 30 days advance notice of the need for leave, when the leave is foreseeable. When not
foreseeable, a resident/fellow must notify CAHC as soon as practicable, and certainly within two (2)
business days of learning of the need for leave, except in extraordinary circumstances. Notice of the need
for leave should be provided to [email protected].
When possible, the resident/fellow is required to provide their Program Director and the Capital Area
Health Consortium with at least two weeks’ advance notice of the date the resident/fellow intends to return
to training. When a resident/fellow returns from family/parental leave, the Program Director, in
consultation with the GME Office, will determine the resident’s/fellow’s status in the program specifically
as it relates to an extension of training and whether the resident/fellow may return to their previous level
of training (see Contract Extension Due to Leave Guidelines Policy).
If a resident/fellow fails to report to work promptly at the end of the family/parental leave, their
appointment with the UConn SOM and their employment with the CAHC may be terminated.
If a resident/fellow is unable to return to training after 12 weeks of family/parental leave, they must
contact CAHC, their Program Director, and the Office of Graduate Medical Education as soon as possible.
The status of a resident/fellow unable to return to training after 12 weeks of family/parental leave will be
determined by the Program Director in consultation with the GME Office. The position of the
resident/fellow may or may not be held.
Taking any leave may extend the time necessary to complete the program requirements for graduation as
well as Board eligibility (see Contract Extension Due to Leave Guidelines Policy). Residents/fellows are
responsible for understanding their Residency Review Committee/Program requirements for program
completion as well as their Board requirements regarding Board eligibility, specifically as it relates to time
away from their program.
Revised 4/19, 10/20, 5/21, 11/21, 12/21, 2/22, 5/22, 1/23, 8/23, 10/23, 6/24
Reviewed 3/21
145
Residents/Fellows Policies and Procedures Manual
MILITARY LEAVE
Military Leaves are available to residents/fellows who have been employed for 3 months or more and
require time off to address qualifying exigency, to care for a military family member who is injured during
active duty, or to care for a veteran with a serious illness as defined under Connecticut law. Residents and
fellows eligible for military leave are eligible for CT Family and Medical Leave and may also be eligible for
Federal Family and Medical Leave. Residents/Fellows may also be eligible for GME leave (see GME One-
Time Leave Policy) and CT Paid Leave benefits administered by CAHC’s private plan (see CT Family and
Medical Leaves of Absence (CTFMLA), Federal Family and Medical Leave (FMLA) and CT Paid Family and
Medical Leaves of Absence (CTPFML) Policy). Available leaves will run concurrently. Military leave
eligibility requires leave paperwork verifying the need for leave and its beginning and expected end dates.
Residents/Fellows are required to use their available vacation time prior to receiving any paid leave
benefits under CAHC’s private plan. Employees can reserve two weeks of vacation time for future use if
available at the time of leave.
Once available vacation and GME leave time is exhausted, a resident/fellow may be eligible to receive CT
Paid Leave benefits administered by CAHC’s private plan. This leave falls under family leave and will be
paid in accordance with the State’s benefit rate after GME leave time is exhausted, which is capped at 60
times the minimum wage rate for the remaining period of absence (not to exceed 12 weeks or 84 days in a
twelve-month period). A resident/fellow may elect to use the reserved vacation time to supplement the
State’s rate cap and receive full pay if a request is submitted to CAHC in writing. Military leaves extending
past 12 weeks will be unpaid.
Residents/fellows who have been employed for less than 3 months and who are in need of a military
caregiver leave or to attend to specific issues associated with a qualifying exigency, to care for a military
family member who is injured during active duty, or to care for a veteran with a serious illness are eligible
for GME leave and must comply with the requirements of the GME One-Time Leave Bank Policy (see GME
One-Time Leave Bank Policy). Four weeks of vacation is available to residents/fellows on the first day of
employment, and must be used during the GME leave.
Employees can reserve two weeks of vacation time for future use if available at the time of leave.
Residents/fellows may also be eligible for CT Paid Leave benefits administered by CAHC’s private plan (see
CT Family and Medical Leaves of Absence (CTFMLA), Federal Family and Medical Leave (FMLA) and CT
Paid Family and Medical Leaves of Absence (CTPFML) Policy). Additional military caregiver leave taken
after the GME leave is exhausted will be unpaid unless CT Paid Leave eligibility requirements are met.
Residents/fellows must submit the necessary paperwork (including a treating physician certification in
the case of a leave to care for a current member of the armed forces who suffered a serious injury or illness
in the line of duty, or a veteran with a serious illness) to support their leave request and return to the
Capital Area Health Consortium.
When possible, the resident/fellow is required to provide their Program Director and the Capital Area
Health Consortium with at least two weeks advance notice of the date the resident/fellow intends to return
to training. When a resident/fellow returns from military leave, the Program Director in consultation with
the GME Office will determine the resident’s/fellow’s status in the program specifically as it relates to
146
Residents/Fellows Policies and Procedures Manual
extension of training and whether the resident/fellow may return to their previous level of training (see
Contract Extension Due to Leave Guidelines Policy).
To the extent applicable, any family/military leave, GME leave, CT Family and Medical Leave,
Federal Family and Medical Leave and CT Paid Leave will run concurrently.
If a resident/fellow fails to report to work promptly at the end of the military leave, their appointment with
the UConn SOM and their employment with the CAHC may be terminated.
If a resident/fellow is unable to return to training after 26 weeks of military family leave, they must contact
CAHC, their Program Director and the Office of Graduate Medical Education as soon as possible.
The status of a resident/fellow who is unable to return to training after 26 weeks of military leave will be
determined by the Program Director in consultation with the GME Office. The position of the
resident/fellow may or may not be held.
Taking any leave may extend the time necessary to complete the program requirements for graduation as
well as Board eligibility (see Contract Extension Due to Leave Guidelines Policy). Residents/fellows are
responsible for understanding their Residency Review Committee/Program requirements for program
completion as well as their Board requirements regarding Board eligibility, specifically as it relates to time
away from their program.
If, during the course of training and employment, a resident/fellow volunteers for military service (not as
a non-military contractor or employee), fulfills military training requirements, is required to serve active
duty, required to perform training, or required to provide emergency services in the Armed Forces of the
United States, the resident/fellow and the spouse of a military service person shall be granted a leave of
absence from the program and employment in accordance with the law. Further, in accordance with the
law, the resident/fellow shall have employment, training, and reemployment rights in accordance with the
requirements of state and/or federal law, including the Uniformed Services Employment and
Reemployment Rights Act, as amended, and/or regulations issued thereunder, and the U.S. and Connecticut
Family and Medical Leave Acts, consistent with program requirements and accreditation standards. This
includes any rights to Federally-recognized spousal or military reserve leaves. The resident/fellow or
spouse shall have no right to additional compensation or benefits, except as required by law.
Taking any leave (especially when multiple leaves or absences occur in the same contract year) may extend
the time necessary to complete the program requirements for graduation as well as for Board eligibility
(see Contract Extension Due to Leave Guidelines Policy). Residents/fellows are responsible for
understanding their Residency Review Committee/Program requirements for program completion as well
as their Board requirements regarding Board eligibility, specifically as it relates to time away from their
program.
Any and all leaves must be approved by the Program Director.
Revised 12/21, 5/22, 1/23, 8/23, 10/23, 6/24
Reviewed 3/16, 3/17, 5/17, 4/19, 3/21

147
Residents/Fellows Policies and Procedures Manual
EMERGENCY LEAVE
Emergency leave with pay and benefits may be granted under certain circumstances that are beyond the
resident’s/fellow’s control and that do not qualify for another leave reason. A resident/fellow must
communicate with the Program Director or designee to request an emergency leave. The resident/fellow
granted emergency leave is required to communicate with the Program Director or designee within 48
hours of the approved request to discuss his/her status in the program. If the resident/fellow does not
communicate with the Program Director, the appointment letter/contract and employment with CAHC
may be considered terminated.
Emergency leave should not be longer than 7 consecutive days. If additional time is needed, another leave
status must be obtained.
A resident/fellow’s time in the program may be extended to meet all requirements of the
residency/fellowship program and board certification. Determining whether emergency leave will reduce
sick time and vacation time and/or if an extension is needed will be at the discretion of the Program
Director with consultation with the GME Office.
Revised 6/24
Reviewed 3/16, 5/17, 4/19, 3/21, 9/21, 2/23, 10/23
148
Residents/Fellows Policies and Procedures Manual
BEREAVEMENT LEAVE
In the event of a family member’s death, a resident/fellow, may take bereavement leave of up to three
consecutive workdays with pay. Immediate family is defined as parents, parents-in-law, siblings,
spouse/domestic partner, children, grandparents, grandchildren, or an individual related to the employee
by blood or affinity and whose close association to the employee shows to be the equivalent of those family
relationships. Qualified bereavement leave does not reduce vacation time or sick days. Bereavement leave
must be approved by the Program Director.
Taking any leave (especially when multiple leaves or absences occur in the same contract year) may extend
time necessary to complete the program requirements for graduation as well as for Board eligibility (see
Contract Extension Due to Leave Guidelines Policy). Residents/fellows are responsible for understanding
their Residency Review Committee/Program requirements for program completion as well as their Board
requirements regarding Board eligibility, specifically as it relates to time away from their program.
Revised 12/21, 1/23, 10/23
Reviewed 3/16, 3/17, 4/17, 5/17, 4/19, 3/21

149
Residents/Fellows Policies and Procedures Manual
PERSONAL LEAVE
Under certain circumstances, a resident/fellow may request an unpaid personal leave of absence for any
reason not covered by another leave policy or after another leave ends and if the resident/fellow has
exhausted or is not eligible to receive sick or vacation time.
A personal leave request must be approved by the Program Director. Unlike other leaves, which are
required by law (family and medical, jury duty, military) a personal leave is at the sole discretion of the
Program Director in consultation with the GME Office. The Program Director will take into consideration
the reason for the leave, prior leaves, the needs of the program, as well as the length of the leave, in
deciding if a leave will be granted and for how long. The Program Director will be responsible for
informing the GME Office and the Capital Area Health Consortium if a personal leave request has been
approved.
A resident/fellow who requests and is granted an unpaid personal leave must contact the Capital Area
Health Consortium regarding pay and benefits while on personal leave. The resident/fellow will not
receive pay for the duration of said leave. Benefits that have not already been discontinued will continue
for up to 30 days at the resident’s/fellow’s own cost. The resident/fellow will need to reimburse the
Consortium for the benefit payroll deduction for the personal leave taken. After 30 days, there is an
option for continuation of coverage through COBRA. The Capital Area Health Consortium will provide the
cost of coverage to the resident/fellow.
When a resident/fellow requests such a leave of absence, the resident’s/fellow’s position may or may
not be held.
Should a resident/fellow take an unpaid leave of absence without appropriate notification and approval
by the Program Director, the resident’s/fellow’s appointment with the UConn SOM and employment with
the CAHC may be considered terminated.
Taking any leave (especially when multiple leaves or absences occur in the same contract year) may
extend time necessary to complete the program requirements for graduation as well as for Board
eligibility (see Contract Extension Due to Leave Guidelines Policy). Any personal leave that goes beyond
12 weeks could result in the termination of the appointment with UConn SOM and the end of
employment with CAHC. Residents/fellows are responsible for understanding their Residency Review
Committee/Program requirements for program completion as well as their Board requirements
regarding Board eligibility, specifically as it relates to time away from their program.
Revised 3/16, 3/17, 5/17, 4/19, 10/20, 3/21, 12/21, 5/23
Reviewed 2/23

150
Residents/Fellows Policies and Procedures Manual
CONTRACT EXTENSION DUE TO LEAVE GUIDELINES
Continuous and complete training is vital to residents/fellows in all disciplines. If a resident/fellow is on
leave for any approved reason and requires extended time away from training such that the
resident/fellow is unable to satisfy the academic and curricular requirements of the program within the
time allotted, the Program Director will need to determine the extent to which the resident/fellow’s
educational experience was interrupted by time on leave. Once that is determined, the Program Director
will need to decide the outcome for that individual resident/fellow and the impact the leave had on the
integrity of the learning process and training program. Possible outcomes include extension of training
equal to the amount of training lost; extension of training longer than the amount lost on leave including
repeating a full year of training; and lastly non-renewal of contract. The Program Director will take into
consideration the full impact associated with discontinuous training for the individual resident/fellow i.e.,
whether the resident/fellow is meeting program and specialty standards. In all situations, the Program
Director must consult with the GME Office prior to determining the appropriate outcome.
Extension of time granted by the Program Director in consultation with the GME Office may take into
consideration the spectrum of specialty board requirements, RC requirements, program requirements, and
institutional requirements. Vacation granted during an extension will vary and depend on the amount of
extension required to complete the requirements of training. If extension is greater than 3 months, vacation
and sick time will be prorated for the period of extension.
Reviewed 3/16, 3/17, 5/17, 4/19, 3/21, 2/23

151
Residents/Fellows Policies and Procedures Manual
RESTRICTED COVENANT
In compliance with Accreditation Council for Graduate Medical Education (ACGME) requirements, neither
the University of Connecticut School of Medicine (UConn SOM) nor any of its Graduate Medical Education
(GME) programs will enter into a non-compete arrangement or other restrictive covenant with any
resident/fellow.
Reviewed 3/15, 5/17, 4/19, 3/21, 2/23

152
Residents/Fellows Policies and Procedures Manual
CLOSURES AND REDUCTIONS IN PROGRAMS AND PROGRAM SIZE
If UConn SOM, the sponsoring institution, decides to close, ACGME will be notified. The GMEC, Associate
Dean for GME, Designated Institutional Official, Program Directors, and residents/fellows will all be
notified immediately. The UConn SOM will, whenever possible, allow residents/fellows already enrolled in
programs
to complete their education. If it is not possible for a resident/fellow to complete their education
at the UConn SOM, the Program Director will assist the residents/fellows in enrolling in another program
in which they may complete their education. In the unlikely event that this occurs, the
process for each
sponsored program will be outlined and posted on HuskyCT.
Reviewed 3/16, 5/17, 3/21, 2/23

153
Residents/Fellows Policies and Procedures Manual
EXTRAORDINARY CIRCUMSTANCES GUIDELINES
INCLUDING DISASTERS OR EXTREME EMERGENT SITUATIONS
The University of Connecticut is committed to preserving the educational experiences of its
residents/fellows during times of extraordinary circumstances. Extraordinary circumstances include but
are not limited to abrupt hospital closure, a natural disaster, or a catastrophic loss of funding.
If the Extraordinary Circumstances policy is invoked, the Designated Institutional Official (DIO), or
designee(s), on behalf of the affected Sponsoring Institution will:
• Provide a plan describing the continuation of residents’/fellows’ educational experiences and any
major changes to the Sponsoring Institution and its programs
• Arrange timely reassignment of residents and fellows, including their temporary or permanent
transfers to other ACGME-accredited programs as needed to ensure they can continue their
education
• Ensure that residents and fellows are prospectively informed of the estimated duration of any
temporary transfer to another ACGME-accredited program
• Ensure that residents/fellows continually receive timely information regarding reassignments,
transfer arrangements, and/or major changes to the Sponsoring Institution or its programs
Residents/fellows are required to keep open channels of communication by phone or email during an
extraordinary circumstance and particularly during an extreme emergency or disaster in order to keep
informed of current and updated information.
The Sponsoring Institution will make every effort to ensure that there is no interruption in the salary and
benefits provided to a resident/fellow once an extraordinary circumstance has been declared.
Reviewed 3/15, 5/17, 4/19, 3/21
Revised 2/23

154
Residents/Fellows Policies and Procedures Manual
SECTION VI: GENERAL INFORMATION AND
SUPPORT SERVICES

155
Residents/Fellows Policies and Procedures Manual
REPORTING CONCERNS
The University of Connecticut (UConn) School of Medicine (SOM) is committed to fostering an environment
where residents and fellows feel comfortable raising concerns. To that end, multiple avenues to report
concerns are available.
Faculty
Residents/fellows may report any concerns they have about their training program to any one or to all of
the following individuals: the Program Director, a core faculty member, the Department Chair, the Office
of Graduate Medical Education (specifically the Designated Institutional Official, the Assistant Designated
Institutional Official, and/or the Associate Dean for Graduate Medical Education) and the Dean of the
School of Medicine.
GME Hotline:
Residents/fellows may report any concerns they have about their training program through the GME
Hotline phone number or through the GME Hotline email. Faculty and staff who work with
residents/fellows may also use the GME Hotline to report concerns.
• GME Hotline phone number: 860-679-4353
• GME Hotline email: gmehotline@uchc.edu
Reporting of concerns through the Hotline phone number may remain anonymous. The individual
reporting the concern may identify themselves if comfortable doing so. Given the nature of email
communications, in general, reporting of concerns though the GME Hotline email is not anonymous unless
an email address is used which does not reveal the identity of the sender.
To help the GME Office appropriately and thoroughly review and, where appropriate, respond to the
concern, it is helpful for the individual reporting the concern to provide as much information as they are
comfortable providing. This includes but is not limited to specific information about the concern or
incident, training program, site, date, and name of any involved persons.
Office of University Compliance:
Residents/fellows may report concerns to the University of Connecticut’s Office of University Compliance
REPORTLINE. The REPORTLINE is supported by a third-party vendor and staffed by professionals. It
serves as an anonymous resource for residents/fellows to report concerns by phone or by an online
webform.
• (REPORTLINE phone number: 1-888-685-2637)
• (REPORTLINE online form: https://compliance.uconn.edu/reporting-concerns/reporting-
overview/)
Office of Institutional Equity (OIE):
The Office of Institutional Equity (OIE) receives reports concerning alleged Prohibited Conduct pursuant
to the Policy Against Discrimination, Harassment and Related Interpersonal Violence. Residents/fellows
may use the OIE’s online form to report concerns regarding Prohibited Conduct under the Policy, whether
156
Residents/Fellows Policies and Procedures Manual
the report is regarding an individual’s own concerns, or a report is being made pursuant to the responsible
employee reporting responsibilities set forth in the Policy, including those specific to student disclosures
of sexual assault, intimate partner violence and stalking.
• OIE Reporting Form: https://equity.uconn.edu/reporting-form/
Revised 8/17, 4/19, 1/21, 3/21

157
Residents/Fellows Policies and Procedures Manual
AWAY ELECTIVES
An away elective, be it clinical or research-based, is a rotation at an institution that is not affiliated with
the
University of Connecticut School of Medicine (UConn SOM), where the resident/fellow is not directly
supervised and evaluated by a UConn SOM faculty member. The Graduate Medical Education (GME)
Office
designee will determine the merits of the request for an away elective and be responsible for approval
(when necessary) of resident/fellow participation.
Away electives with prior approval NOT required
If a resident/fellow is participating in an away elective to fulfill an ACGME program requirement that
cannot be accomplished at UConn, specific approval by the GME Office is not required. However,
residents/fellows will still be required to complete and submit all appropriate away elective
paperwork to the GME Office.
Away electives with prior approval required
Residents/fellows may apply for approval for away electives for clinical or research experiences.
Program Director approval for such away electives must be obtained by the resident/fellow prior to
the resident/fellow applying for approval from the GME Office.
An Away Elective Form must be completed and is available on the GME website:
Away Elective
Application Essential components of the necessary
paperwork include:
• Educational rationale for requesting an away elective
• Program Director’s support for this experience
• Evaluation tool used to evaluate the resident/fellow’s experience
• Program’s effort to identify funding support for this experience
• ECFMG’s offsite rotation notification form (if applicable)
Away electives outside of the United States are typically approved when the experience is done in
conjunction with a School of Medicine faculty member, or at a site with a pre-established relationship
between the School of Medicine or a faculty member. Other international electives will be reviewed on a
case-by-case basis with a focus on resident safety, the educational experience based on rotational goals and
objectives, availability of appropriate supervision, and an appropriate evaluation tool for the experience.
A resident/fellow who is not in good standing in their training program may not participate in
an away
elective. A resident applying for an away elective should not make any travel arrangements until they
receive approval from the GME Office.
Expenses incurred for required vaccinations and appropriate travel medications related to an approved
international away elective will be covered if incurred at the UConn Health travel clinic. The
resident/fellow may be liable for any out-of-pocket expenses incurred elsewhere.
Typically, a resident/fellow is only permitted 1 away elective experience during each UConn sponsored
training program matriculated in.
Revised 12/17, 2/18, 4/19, 3/21
Reviewed 3/16, 4/17, 3/21

158
Residents/Fellows Policies and Procedures Manual
OFFICIAL COMMUNICATION WITH THE UNIVERSITY OF CONNECTICUT SCHOOL OF
MEDICINE GRADUATE MEDICAL EDUCATION PROGRAMS
All residents/fellows are required to monitor and use their University of Connecticut School of Medicine
(UConn SOM) endorsed email accounts. Monitoring of the professional email account must occur at least
weekly to guarantee that all correspondence is reviewed. Any correspondence with the staff in the UConn
SOM GME Office or the CAHC for any work-related issues must be conducted through these accounts. A
program’s communication policy may require more frequent monitoring. Please refer to the program's
manual.
Reviewed 3/15, 5/17, 4/19, 3/21, 2/23
159
Residents/Fellows Policies and Procedures Manual
MEDICAL TREATMENT/PRESCRIPTION WRITING
Residents/fellows may provide treatment for patients they are caring for on their assigned rotations, both
inpatient and outpatient. Such treatment may include but is not limited to providing direct clinical care,
writing prescriptions, ordering tests, or making referrals.
Connecticut requires several numbers before these privileges are available. Please refer to National
Provider Identifier (NPI) Number, Connecticut Controlled Substance Number, Connecticut Prescription
Monitoring and Reporting System (CPMRS), and Drug Enforcement Administration (DEA) Number for
more information on what is required.
A resident/fellow who provides treatment for someone who is not under his/her care as part of the
residency/fellowship program, is NOT covered by malpractice liability. This activity is prohibited. The
resident/fellow who engages in this activity may be subject to disciplinary action.
Revised 3/16, 5/17, 4/19, 3/21
Reviewed 2/23

160
Residents/Fellows Policies and Procedures Manual
PROVIDING MEDICAL TREATMENT TO RESIDENTS/FELLOWS
Residents/fellows may choose to seek medical care by faculty members at the University of Connecticut or
any of its affiliated hospitals or ambulatory sites. It is the purpose of this policy to provide guidelines to
our residents/fellows in order to protect the resident’s/fellow’s right to privacy, as well as to preserve the
integrity of the faculty/trainee educational relationship.
Residents/fellows who are seeking medical care should strongly consider obtaining that care from
physicians who are not faculty members with authority over them as trainees. Faculty members with
authority over a resident/fellow include, but are not limited to, faculty members who provide teaching,
supervision of clinical duties, formal mentoring, supervision of research, and evaluation to the
resident/fellow.
If a resident/fellow needs advice regarding this policy, they should contact the GME Office.
Revised 3/21
Reviewed 3/15, 5/17, 4/19, 2/23

161
Residents/Fellows Policies and Procedures Manual
JURY DUTY
Participation in jury duty is a civic responsibility. If a resident/fellow gets called for jury duty, they must
notify the program director or designee. The Program Director must make arrangements to release the
resident/fellow from clinical activities during the jury duty process. If a resident/fellow participates in jury
duty, a copy of their juror certificate indicating their dates of service as a juror must be submitted to their
program office and CAHC promptly to be properly compensated. Residents/fellows will receive full pay
and benefits during this time.
Taking any leave (especially when multiple leaves or absences occur in the same contract year) may
negatively impact time necessary to complete the program requirements for graduation as well as for
Board eligibility (see Contract Extension Due to Leave Guidelines Policy). Residents/fellows are
responsible for understanding their Residency Review Committee/Program requirements for program
completion as well as their Board requirements regarding Board eligibility, specifically as it relates to time
away from their program.
Reviewed 3/16, 3/17, 5/17, 4/19, 3/21, 2/23
162
Residents/Fellows Policies and Procedures Manual
SECURITY
Security measures are provided within the University of Connecticut School of Medicine, the sponsoring
institution, as well as all of the major affiliated hospitals, including the UConn Health, Hartford Hospital, St.
Francis Hospital and Medical Center, Hospital for Central Connecticut, Connecticut Children’s Medical
Center, and the Veterans’ Administration. These include foot and vehicle patrol of the facilities and general
response to problems that arise. Security also provides assistance with ambulance security, transportation
of patients to and from aircraft sent to the hospital, unlocking doors, escorts to vehicles, and assistance
with cars that will not start in the middle of the night.
Operator Phone Numbers
UConn Health (860) 679-2000
Hartford Hospital (860) 545-5000
St. Francis Hospital & Medical Center (860) 714-4000
Hospital of Central Connecticut - New Britain Campus (860) 224-5011
Connecticut Children’s Medical Center (860) 545-9000
Veteran’s Administration - Newington (860) 666-6951
Security/Public Safety Office Phone Numbers
UConn Health (860) 679-2121
Hartford Hospital (860) 545-2147
St. Francis Hospital & Medical Center (860) 714-4492
Hospital of Central Connecticut - New Britain Campus (860) 224-5107
Connecticut Children’s Medical Center (860) 545-2147
Veteran’s Administration - Newington (860) 666-6951
Revised 2/23
Reviewed 3/15, 5/17, 4/19, 3/21

163
Residents/Fellows Policies and Procedures Manual
BEEPERS
Residents/fellows may be provided a beeper during their appointment period. Beepers must be
returned upon completion of training. If a resident/fellow is remaining at UConn Health after
completion of the program, the beeper must be returned, or the new department must change the
funding account with the Telecommunication Department.
SECURE ELECTRONIC MESSAGING
TigerConnect and Voalte are systems that have been provided to residents/fellows in order to ensure a
secure, HIPAA-compliant means of communication about patient care. TigerConnect or Voalte can be
accessed through an app at the App Store (Apple) or Google Play (Android). Additional information is
available in the “GME Updates for Residents and Fellows” organization on HuskyCT.
MEAL ALLOWANCE
A meal allowance of $15 per shift is added to the resident’s/fellow’s stipend for each shift they are on “in-
house” call in excess of 14 hours as reported by the program leadership. This is disbursed quarterly by
CAHC through a post-tax addition to their paycheck. In addition to the meal allowance, there is 24-hour
access to food at any site at which the resident/fellow has overnight call.
Revised 3/16, 5/17, 11/17, 2/23, 6/24
Reviewed 4/19, 3/21

164
Residents/Fellows Policies and Procedures Manual
HOLIDAY GUIDELINES
Residents/fellows may be scheduled and required to work on holidays in order to provide adequate patient
coverage. Individual programs will be responsible for scheduling residents/fellows on holidays.
Residents/fellows should refer to their specific program’s policy regarding holiday work schedules.
Revised 3/16, 3/17
Reviewed 4/19, 3/21, 1/23

165
Residents/Fellows Policies and Procedures Manual
INCLEMENT WEATHER
Residents/fellows are essential to the daily operation of each hospital and are expected to report to work
when scheduled. In the event of a severe weather condition such as a snowstorm, residents/fellows must
contact their Program Director and supervisor to determine staffing needs. In some cases, outpatient
activities may be cancelled or delayed, and residents/fellows may be temporarily re-assigned to help the
inpatient demands. Prior to their assigned shift each resident/fellow should contact their Program Director
and supervisor to determine where and if they are needed. Residents/fellows should plan for extra travel
time when proceeding to and from their assigned locations. In some events, residents/fellows may be
needed to stay past the end of an assigned shift to ensure patient safety until appropriate staffing can be
assured. Every effort will be made to establish designated rest areas for residents/fellows required to stay
beyond their assigned shift. If a resident/fellow is unable to arrive for a shift on time, they should contact
their supervisor immediately.
Revised 3/15, 5/17
Reviewed 4/19, 3/21, 2/23

166
Residents/Fellows Policies and Procedures Manual
NEEDLESTICKS & OTHER OCCUPATIONAL EXPOSURE TO BLOODBORNE PATHOGENS
Residents/fellows who experience a needlestick or occupational exposure to bloodborne pathogens are
required to follow the guidelines listed below:
Wear procedure work related injury “purple card” on their badges at all times.
Immediately present “purple card” at point of care.
Notify their supervisor of an accident or injury occurring while on the job.
Keep their supervisor informed of their medical status on an on-going basis.
Follow the physician’s treatment plan.
Keep medical appointments and avoid any activity which will further aggravate the injury.
Accident or Injury Information
During the day, the resident/fellow must go to the site’s Employee Health Department.
Off-hours the resident/fellow should go to the Emergency Room of the working site.
• If at Connecticut Children’s Medical Center (Connecticut Children’s), go to Hartford Hospital’s
Emergency Room.
The incident must also be reported by the resident/fellow to the Capital Area Health Consortium.
• During the day, this must be done immediately following initial treatment (preferably while at
the Employee Health Department at the hospital).
• If off-hours, a message with the resident’s/fellow’s contact number must be left.
Blood-Borne Pathogen Training
All residents/fellows are required to receive an annual training in blood-borne pathogens. The initial
training is done at orientation for all new residents/fellows. The annual training renewal is part of the
Institutional Curriculum requirements. The training is through the HealthStream web-based courses.
Revised 3/15, 5/17, 2/18
Reviewed 4/19, 3/21, 2/23
